Very long-chain fatty acids (VLCFAs), defined as fatty acid species exceeding 22 carbon atoms, undergo primary metabolism via the peroxisomal β-oxidation pathway in humans. These lipids exhibit distinctive physiological characteristics: they serve as fundamental constituents of phospholipid membranes (particularly within neuronal myelin structures) while simultaneously functioning as signaling molecules critical for nervous system development and regulation. Within neural tissues, VLCFAs predominantly localize to two essential lipid classes:
- Sphingomyelins (e.g., 28-34 carbon polyunsaturated species)
- Glycerophospholipids (notably C24-C36 disaturated phosphatidylcholines uniquely present in retinal tissue)
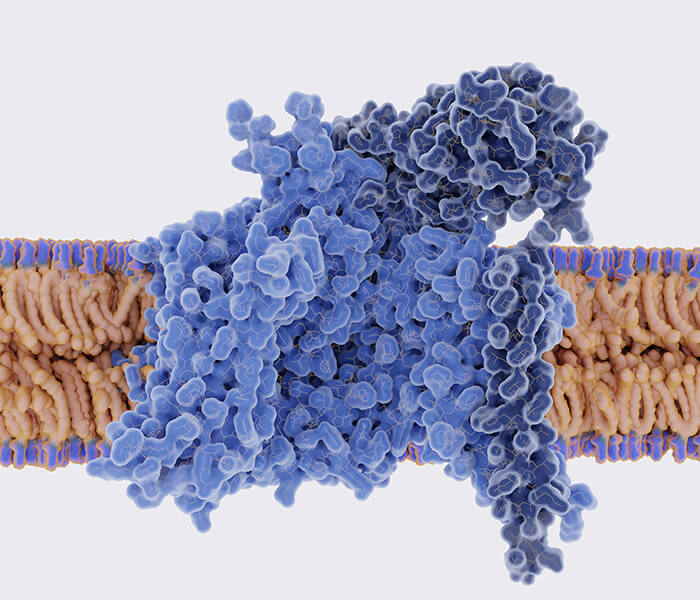
 Role of ELOVL1 in X-ALD and other neurological diseases (Siddiqui AJ et al., 2023)
Role of ELOVL1 in X-ALD and other neurological diseases (Siddiqui AJ et al., 2023)
Dysregulation of these specialized lipids demonstrates strong associations with neurodegenerative pathologies including X-linked adrenoleukodystrophy (X-ALD), multiple sclerosis (MS), and Alzheimer's disease (AD). Metabolomics advancements now enable comprehensive investigation of VLCFA mechanisms in neurological disorders. Contemporary analytical platforms integrate high-resolution mass spectrometry (e.g., Orbitrap Fusion Lumos) with chromatographic separation techniques (HILIC and RP-LC), permitting precise quantification of VLCFAs and derivatives in minute biological specimens (<0.5 μL). This integrated approach delivers three principal advantages:
- Comprehensive metabolite profiling: Simultaneous detection of hundreds of lipids enables reconstruction of complete metabolic networks
- Structural discrimination: ppm-level mass accuracy resolves structurally analogous VLCFA isomers
- Ultra-trace sensitivity: Femtogram-level detection facilitates lipidomic analysis of microsamples (e.g., single organelles or CSF)
Services You May Be Interested In:
2 Core Case 1: Discovery of the VLCFA-S1P Pathway in Glial Cells
2.1 Research Design and Methodological Innovation
- Employing a collaborative Drosophila-mouse model integrated with multi-omics analysis, this study addresses three key questions:
- What is the metabolic fate of VLCFAs leading to neurotoxic sphingolipid production within glial cells?
- How do these toxic lipids impair neuronal function?
- Is therapeutic intervention in this pathway viable for demyelinating disorders?
- Precision genetic manipulation underpinned model development:
- Drosophila: CRISPR/Cas9 generated glial-specific strains (dACOX1 knockout, ELOVL1 overexpression).
- Mouse: Experimental autoimmune encephalomyelitis (EAE) modeled human multiple sclerosis.
- Cell: Primary astrocytes with TMEM164 overexpression via adeno-associated virus.
- Lipidomics featured innovative breakthroughs:
- Nano electrospray-high resolution mass spectrometry (nanoESI-HRMS) tracked VLCFA metabolic flux.
- An MS³ cascade fragmentation strategy precisely identified ω-hydroxyl positions (C18 vs C24).
- Dual-mode analysis complemented detection: positive ion mode for [M+Na]⁺ adducts and negative ion mode for [M-H]⁻ fragments.
- Multidimensional behavioral and pathological assessments were implemented:
- Neural Function: Drosophila climbing tests (motor), lifespan analysis (survival).
- Electrophysiology: Electroretinograms recorded neuronal activity.
- Histopathology: Myelin integrity (LFB staining), axon loss (neurofilament staining).
- Immunoinflammation: Glial activation markers (Iba1/CD8), CNS macrophage infiltration quantification.
2.2 Core Findings and Mechanism Analysis
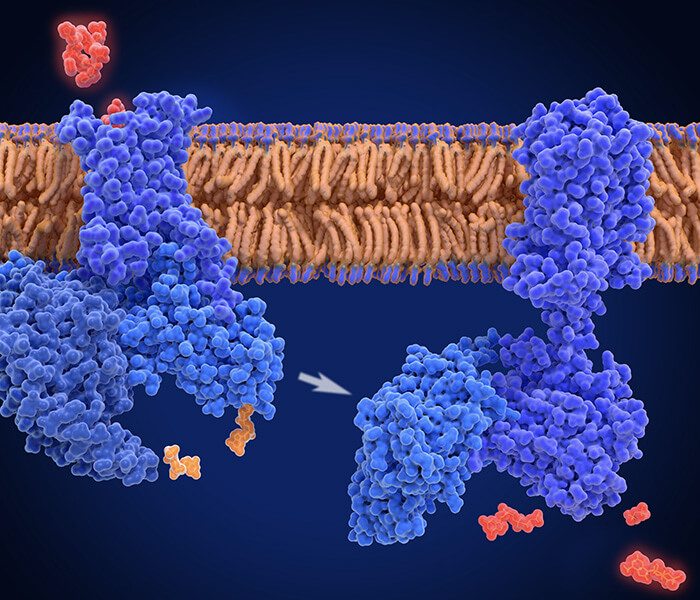
- The research revealed that VLCFA accumulation in glia activates a novel "S1P export pathway":
- ELOVL enzymes elongate VLCFA chains (primarily generating C32:1/C34:1 species).
- Elongated VLCFAs convert into very long chain ceramides (VL-Ceramide).
- Sequential catalysis by CDase and SK1 enzymes synthesizes sphingosine-1-phosphate (S1P).
- This pathway mediates dual neurotoxicity:
- Neurophagocytosis: S1P upregulates the phagocytic receptor Draper, promoting aberrant glial engulfment of neurons.
- Neuroinflammatory Cascade: S1P triggers the IMD immune pathway, elevating antimicrobial peptide gene expression and inducing CNS macrophage infiltration.
Molecular imaging confirmed S1P transcellular transport: Fluorescent S1P signals intensified 3.8-fold (p<0.001) in neuronal regions of Drosophila brains with glial ELOVL1 overexpression, evidencing "glial-to-neuronal" transit.
2.3 Treatment Strategies and Intervention Effects
- Mechanistic insights led to the proposal and validation of a dual-target therapeutic approach:
- Target 1: VLCFA synthesis (Bezafibrate activates peroxisomal β-oxidation).
- Target 2: S1P signaling (Fingolimod downregulates S1P receptors).
- Significant efficacy was observed in the EAE model:
- Monotherapy: Bezafibrate reduced clinical scores by 40%; Fingolimod by 45%.
- Combination Therapy: Clinical scores decreased 78%, demyelination area shrank 85%, and axonal loss diminished 90%.
Table: Comparison of VLCFA-S1P Pathway Targeted Therapy Effects in Neurodegenerative Disease Models
| Treatment Strategy | Motor Function Improvement | Myelin Retention Rate | Neuroinflammation Score | Prolonged Survival |
|---|---|---|---|---|
| Control (normal saline) | 0% | 32.5 ± 4.2% | 8.2 ± 0.7 | 0 days |
| Bezafibrate monotherapy | 41.3 ± 5.1%* | 67.8 ± 5.1%* | 4.5 ± 0.5* | 15.3 ± 2.1 days* |
| Fingolimod monotherapy | 46.2 ± 4.7%* | 63.5 ± 4.8%* | 4.1 ± 0.6* | 17.6 ± 2.4 days* |
| Double-drug combination | 82.7 ± 6.3%** | 89.4 ± 3.7%** | 1.8 ± 0.4** | 32.7 ± 3.5 days** |
(*p<0.01 vs control; **p<0.001 vs monotherapy; data source)
This work establishes the pivotal role of the VLCFA-S1P axis in multiple sclerosis and related neurodegenerative diseases, presenting a novel combination target strategy for clinical development (Chung HL et al., 2023).
 Elevated levels of VLCFAs induce S1P production and neuronal dysfunction (Chung HL et al., 2023)
Elevated levels of VLCFAs induce S1P production and neuronal dysfunction (Chung HL et al., 2023)
3 Core Case 2: VLCFA is used to diagnose X-ALD
3.1 Core Diagnostic Limitations of Conventional VLCFA Analysis
- Overlapping Reference Ranges and False Positives: The diagnostic utility of VLCFAs (C24:0, C26:0, and ratios C24:0/C22:0, C26:0/C22:0) is hampered by significant range overlap between healthy individuals and X-ALD patients, leading to elevated false positive rates. Hyperlipidemia, particularly elevated LDL cholesterol, is a primary confounding factor, artificially inflating absolute VLCFA concentrations while leaving ratios unaffected.
- Risk of Missed Diagnosis in Females: Conventional VLCFA testing fails to identify approximately 15% of female carriers (ABCD1 heterozygous mutations) due to normal biomarker levels in these individuals.
3.2 Metabolomic Method Optimization
- Technological Enhancements:
- Standardized Testing: Analysis employed GC-MS coupled with the modified Lepage-Roy method. CIS-13,16,19-DOCOSATRIENOIC acid served as the internal standard, mitigating interference from endogenous serum fatty acids.
- Rigorous Quality Control: Dual-level QC samples (normal/high) ensured precision, achieving a C26:0 coefficient of variation below 9.4% and repeatability errors under 8%.
- Sample Handling: Utilization of fasting serum samples is recommended to minimize triglyceride interference.
- Critical Value Redefinition: Receiver Operating Characteristic (ROC) analysis established optimized diagnostic thresholds:
- C24:0/C22:0: <1.0 (Sensitivity Increase: +6.1%)
- C26:0/C22:0: <0.02 (Sensitivity Increase: +24.2%)
- C26:0: <1.2 μmol/L (Sensitivity Increase: +15.1%)
- Impact: These revised cut-offs substantially enhanced sensitivity (e.g., 90.9% for C26:0/C22:0), though accompanied by a 16.7% rise in false positives. The combined use of both ratios (C24:0/C22:0 + C26:0/C22:0) emerged as the optimal diagnostic strategy.
3.3 Key Findings and Clinical Implications
- VLCFA-Lipid Association: Absolute VLCFA concentrations (C24:0, C26:0) demonstrated a strong positive correlation with LDL cholesterol (p < 0.002), whereas VLCFA ratios remained independent of lipid levels.
- Clinical Recommendation: Co-testing blood lipids is essential. For hyperlipidemic patients, diagnostic interpretation must prioritize ratio analysis to prevent false positives.
- Addressing Gender Disparities:
- Males: VLCFA ratio sensitivity approaches 100%.
- Female Carriers: Due to a 15% miss rate with standard VLCFA testing, ABCD1 gene sequencing remains necessary. The novel biomarker 26:0-lyso-PC, detectable via dried blood spot, increases female carrier identification to nearly 100%.
- Value of Serial Monitoring: Longitudinal testing revealed delayed VLCFA elevation in 10% of initially screen-negative individuals (particularly females), underscoring the need for repeat sampling in high-risk cases.
3.4 Optimized Diagnostic Pathway
For suspected X-ALD
- Perform fasting serum VLCFA testing.
- Employ dual ratio analysis (C24:0/C22:0 + C26:0/C22:0).
- Positive Result: Confirm with ABCD1 gene testing.
- Dyslipidemia Present: Repeat fasting test and prioritize ratio validation.
- Following a negative result in females, supplement with 26:0-lyso-PC analysis or direct ABCD1 genetic testing.
3.5 Future Directions
- Integrate novel biomarkers like 26:0-lyso-PC into routine screening, especially for females and newborns.
- Validate the universality of new critical values through large-scale multicentre studies.
- Investigate the mechanistic role of X-chromosome inactivation skewing on VLCFA expression variability in females.
Summary: This study leverages metabolomic technology to refine VLCFA diagnostic thresholds, significantly boosting X-ALD detection sensitivity. It elucidates the confounding effects of hyperlipidemia and resolves the critical issue of missed female diagnoses. A precision diagnostic strategy combining dual-ratio analysis with genetic testing is proposed. Furthermore, incorporating the novel biomarker 26:0-lyso-PC into clinical practice is advocated to eliminate gender-based diagnostic disparities (Rattay TW et al., 2020).
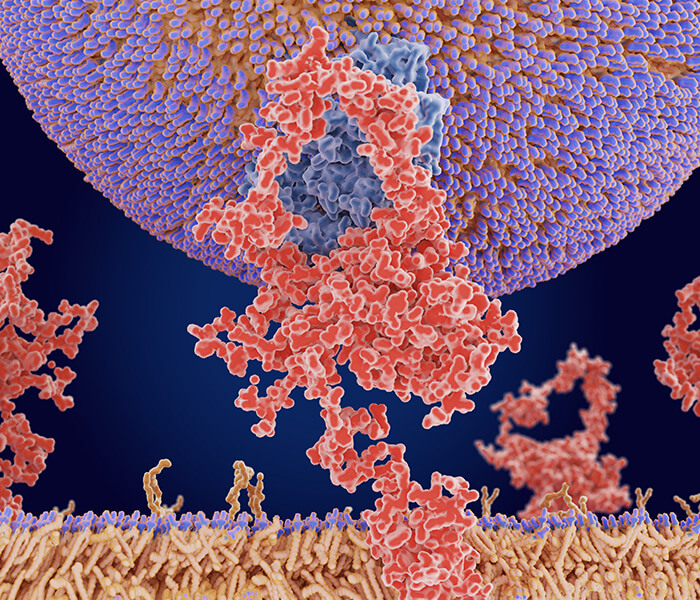
 VLCFA evaluation in phenotypically similar patients (Rattay TW et al., 2020)
VLCFA evaluation in phenotypically similar patients (Rattay TW et al., 2020)
4 Core Case 3:VLCFA metabolomics in frontotemporal dementia (FTD)
4.1 Aberrant VLCFA Metabolism in Frontotemporal Dementia Brains
- Lipid-Specific VLCFA Elevation: Quantitative analysis revealed three significantly elevated VLCFA lipids exclusively in the frontal cortex of FTD patients:
- PC(30:5/18:1)
- PE(33:4/20:4) (novel odd-chain)
- PE(33:4/22:6) (novel odd-chain)
The absence of change in 19 other VLCFA lipids indicates a pathology-specific mechanism.
- ELOVL4-Mediated Synthesis: Upregulated expression of ELOVL4, the key VLCFA synthesis enzyme, positively correlated with FTD progression (higher in late stage). Strong correlations (p < 0.05) between ELOVL4 levels and the three elevated VLCFA lipids confirm its pathogenic role.
- Synaptic Impairment Mechanism: Elevated VLCFA levels directly caused reduced synaptophysin (SYP) expression (mRNA and protein), compromising synaptic vesicle integrity. In vitro validation using ELOVL4-overexpressing neurons confirmed SYP downregulation, demonstrating VLCFA neurotoxicity.
- Impaired Clearance Mechanism: Although ABCD1 transporters (VLCFA efflux pumps) showed compensatory upregulation, their function was severely impaired by profound ATP deficiency (50% reduction in FTD brains). Mitochondrial dysfunction-induced energy crisis thus prevents effective VLCFA clearance.
4.2 Clinical and Biological Implications
- Diagnostic Challenges & Novel Markers: Serum analysis failed to detect elevated brain-specific VLCFA-PC/PE lipids, likely due to blood-brain barrier restriction. This necessitates exploring cerebrospinal fluid (CSF) or imaging biomarkers. Odd-chain VLCFA-PE species represent potential novel FTD-specific markers.
- Pathomechanistic Axis: The core pathology involves: ELOVL4 upregulation → Increased VLCFA synthesis → SYP reduction & synaptic injury + ABCD1 compensatory upregulation → ABCD1 failure due to ATP depletion → VLCFA accumulation. This creates a vicious cycle driving synaptic degeneration.
- Therapeutic Implications:
- Targeting Synthesis: Inhibiting ELOVL4 activity may reduce VLCFA production, but requires careful toxicity balancing (complete loss causes ataxia).
- Joint Strategy: Enhance mitochondrial function to boost ATP supply; Potentiate ABCD1 activity (e.g., via gene therapy).
- Dietary Intervention Ineffective: Brain VLCFAs originate from endogenous synthesis, unaffected by dietary intake.
4.3 Methodological Innovation
- Precision Lipidomics: Employed LC-MS coupled with LipidSearch software for quantitative detection of 22 VLCFA lipids, identifying the 3 specifically elevated species.
- Rigorous Quality Control: Matched human brain tissue and serum analyses minimized batch effects.
- Multi-Level Validation:
- Tissue: Verified protein/mRNA expression via Western blot and qPCR.
- Cellular: SH-SY5Y neuron models (ELOVL4 overexpression/knockdown) confirmed SYP and ABCD1 regulatory relationships.
- Functional: ATP quantification elucidated the energy crisis underlying clearance failure.
4.4 Limitations and Future Directions
- Sample Limitations: Small brain cohort size (n=10 FTD vs. 11 controls) requires validation in larger populations. Seronegative results mandate CSF biomarker exploration.
- Mechanistic Deepening: Clarify the neurotoxicity mechanism of odd-chain VLCFA-PE; Determine why VLCFA specifically impairs SYP but spares other synaptic proteins (e.g., α-synuclein).
- Translational Development: Advance ELOVL4 inhibitor therapeutics; Develop VLCFA-specific imaging probes (e.g., PET tracers).
Summary: This study establishes ELOVL4-driven elevation of specific VLCFA lipids (notably novel odd-chain VLCFA-PEs) as a novel pathological feature in FTD brains. This disrupts synaptic integrity via SYP downregulation and overwhelms clearance mechanisms due to ATP deficiency, creating a degenerative cycle. While serum detection limitations persist, brain VLCFA-PEs offer new diagnostic targets. Therapeutically, the ELOVL4-ABCD1 axis presents intervention points. Future breakthroughs require developing CSF biomarkers combined with strategies targeting brain energy metabolism to overcome current treatment barriers (He Y et al., 2021).
 VLCFA-lipids are increased in FTD brain (He Y et al., 2021)
VLCFA-lipids are increased in FTD brain (He Y et al., 2021)
5. Prospects and Challenges in Clinical Translation of VLCFA Metabolomics
5.1 Diagnostic Implementation Challenges and Strategies
- Translating VLCFA metabolomic profiling into clinical practice faces several critical hurdles:
- Standardization Deficits: Significant inter-laboratory variation exists, with the C24:0/C22:0 ratio differing by up to 18%, critically impacting X-ALD diagnostic accuracy.
- Sample Stability Concerns: Long-term storage compromises integrity, as plasma VLCFA degrades over 15% after 6 months even at -80°C.
- Dynamic Reference Intervals: Age, sex, and dietary factors substantially influence baseline values (e.g., vegetarians exhibit 23% higher C26:0 levels), complicating universal thresholds.
Table: Performance Metrics of VLCFA Biomarkers in Neurological Disorders
| Biomarker | Technology | Cut-off | Sensitivity | Specificity | Clinical Utility |
|---|---|---|---|---|---|
| C24:0/C22:0 ratio | GC-MS/MS | ≥0.15 | 93% | 97% | X-ALD screening |
| S1P (CSF) | UPLC-QTOF | ≥3.2 nM | 87% | 82% | Disease activity assessment |
| VL-ceramide | MALDI-TOF | ≥0.8 μg/ml | 78% | 91% | Treatment response monitoring |
| OAHFA 32:1 | NanoESI-MS | ≤0.15% total lipids | 85% | 89% | Dry eye subtyping |
| PC(16:0/18:1) | HILIC-MS | ≤1.576% (UI) | 83% | - | Neuroinflammation warning |
Mitigation Strategies
- Reference Materials: NIST (USA) is developing SRM 1955, a synthetic CSF with certified VLCFA concentrations.
- Standardized Sampling: Glass capillary collection for tear fluid improves recovery by 14% vs. PTFE tubes, with processing recommended within 4 hours.
- Harmonized Protocols: The IFCC is establishing global VLCFA testing guidelines, slated for 2026 release.
5.2 Personalized Medicine Potential and Barriers
- VLCFA metabolomics holds transformative promise for precision medicine:
- Risk Stratification: ELOVL1 promoter methylation strongly correlates with plasma VLCFA levels (r=0.72), serving as a potential neurodegenerative disease predictor.
- Therapeutic Guidance: FADS2 rs174583 TT-homozygotes show triple the response rate to EPA/DHA fish oil supplementation.
- Real-Time Monitoring: Miniaturized implantable S1P microsensors (0.5mm diameter) enable continuous tracking of neuroinflammation.
- Critical Translational Barriers:
- Economic Constraints: Comprehensive CSF VLCFA profiling costs ~$1,200/test with limited insurance coverage.
- Ethical Considerations: Gene-metabolite interaction analyses raise genetic privacy concerns.
- Implementation Gap: Addressing these challenges necessitates multidisciplinary collaboration across healthcare systems, policymakers, and researchers.
For more on the role of long-chain fatty acids in human disease, read "The Role of Long-Chain Fatty Acids in Human Health and Disease".
For more on the role of Fatty Acidomics in drug discovery see "How Fatty Acid Metabolomics Can Accelerate Your Drug Discovery Pipeline".
The application of fatty acids in microbial research can be consulted "Applications of Fatty Acids Profiling in Microbiome Research".
References
- Siddiqui AJ, Jahan S, Chaturvedi S, Siddiqui MA, Alshahrani MM, Abdelgadir A, Hamadou WS, Saxena J, Sundararaj BK, Snoussi M, Badraoui R, Adnan M. "Therapeutic Role of ELOVL in Neurological Diseases." ACS Omega. 2023 Mar 8;8(11):9764-9774. doi: 10.1021/acsomega.3c00056
- Chung HL, Ye Q, Park YJ, Zuo Z, Mok JW, Kanca O, Tattikota SG, Lu S, Perrimon N, Lee HK, Bellen HJ. "Very-long-chain fatty acids induce glial-derived sphingosine-1-phosphate synthesis, secretion, and neuroinflammation." Cell Metab. 2023 May 2;35(5):855-874.e5. doi: 10.1016/j.cmet.2023.03.022
- Rattay TW, Rautenberg M, Söhn AS, Hengel H, Traschütz A, Röben B, Hayer SN, Schüle R, Wiethoff S, Zeltner L, Haack TB, Cegan A, Schöls L, Schleicher E, Peter A. "Defining diagnostic cutoffs in neurological patients for serum very long chain fatty acids (VLCFA) in genetically confirmed X-Adrenoleukodystrophy." Sci Rep. 2020 Sep 15;10(1):15093. doi: 10.1038/s41598-020-71248-8
- He Y, Phan K, Bhatia S, Pickford R, Fu Y, Yang Y, Hodges JR, Piguet O, Halliday GM, Kim WS. "Increased VLCFA-lipids and ELOVL4 underlie neurodegeneration in frontotemporal dementia." Sci Rep. 2021 Nov 1;11(1):21348. doi: 10.1038/s41598-021-00870-x
- Jaspers YRJ, Yska HAF, Bergner CG, Dijkstra IME, Huffnagel IC, Voermans MMC, Wever E, Salomons GS, Vaz FM, Jongejan A, Hermans J, Tryon RK, Lund TC, Köhler W, Engelen M, Kemp S. "Lipidomic biomarkers in plasma correlate with disease severity in adrenoleukodystrophy." Commun Med (Lond). 2024 Sep 10;4(1):175. doi: 10.1038/s43856-024-00605-9
- Nemeth CL, Gӧk Ö, Tomlinson SN, Sharma A, Moser AB, Kannan S, Kannan RM, Fatemi A. "Targeted Brain Delivery of Dendrimer-4-Phenylbutyrate Ameliorates Neurological Deficits in a Long-Term ABCD1-Deficient Mouse Model of X-Linked Adrenoleukodystrophy." Neurotherapeutics. 2023 Jan;20(1):272-283. doi: 10.1007/s13311-022-01311-x
- Villoria-González A, Zierfuss B, Parzer P, Heuböck E, Zujovic V, Waidhofer-Söllner P, Ponleitner M, Rommer P, Göpfert J, Forss-Petter S, Berger J, Weinhofer I. "Efficacy of HDAC Inhibitors in Driving Peroxisomal β-Oxidation and Immune Responses in Human Macrophages: Implications for Neuroinflammatory Disorders." Biomolecules. 2023 Nov 23;13(12):1696. doi: 10.3390/biom13121696