Long-chain fatty acids (LCFA) are important members of the lipid family and are widely found in many foods in our daily diet, such as vegetable oils, animal fats, and nuts. Their structural characteristics are that they have more than 12 carbon atoms and are usually present in triglycerides composed of glycerol and three fatty acid molecules. Long-chain fatty acids not only provide energy for the human body, but also play a key role in various physiological processes. This article will explore in depth the important role of long-chain fatty acids in human health and disease.
1. Biochemical Foundations and Metabolic Properties of Long-Chain Fatty Acids
1.1 Structural Classification and Physiological Distribution
- LCFAs defined as fatty acids with 12–22 carbon atoms, are categorized by saturation status:
- Saturated (e.g., palmitic acid C16:0)
- Monounsaturated (e.g., oleic acid C18:1)
- Polyunsaturated (e.g., docosahexaenoic acid C22:6)
- Very long-chain fatty acids (VLCFAs; >C22) hold unique biological significance, undergoing primary catabolism via peroxisomal β-oxidation. Within neural tissues, VLCFAs predominantly localize to:
- Sphingomyelins: Containing C28-C34 polyunsaturated species
- Glycerophospholipids: Including retina-specific C24-C36 dipolyunsaturated phosphatidylcholines
Dysregulation of these specialized lipids correlates strongly with neurodegenerative pathologies.
1.2 Metabolic Pathways and Regulatory Control
LCFA homeostasis relies on three interdependent pathways:
- Peroxisomal β-Oxidation:
- Exclusive VLCFA degradation pathway
- Deficiency causes X-linked adrenoleukodystrophy (X-ALD)
- Mitochondrial β-Oxidation:
- Primary energy conversion route for medium/long-chain fatty acids
- Long-chain 3-hydroxyacyl-CoA dehydrogenase (LCHAD) deficiency induces multi-organ damage
- Fatty Acid Elongation:
- Governed by ELOVL (elongase) and KCS (ketoacyl-CoA synthetase) gene families
- Determines fatty acid carbon chain length
- LCFAs exhibit distinct classifications with unique biological properties:
| Classification | Representative Molecules | Primary Food Sources | Key Physiological Functions | Associated Disorders |
|---|---|---|---|---|
| Omega-3 Polyunsaturated Fatty Acids | Docosahexaenoic acid (DHA, C22:6) Eicosapentaenoic acid (EPA, C20:5) | Deep-sea fish Algae | Neural myelination Anti-inflammatory regulation | Cognitive impairment Retinopathy |
| Omega-6 Polyunsaturated Fatty Acids | Arachidonic acid (AA, C20:4) | Vegetable oils Animal meats | Precursor of inflammatory mediators | Cardiovascular diseases Allergic conditions |
| Ultra-Long Chain Saturated Fatty Acids | Nervonic acid (C24:0) | Tree nuts Animal brain tissue | Sphingolipid biosynthesis | Adrenoleukodystrophy (X-ALD) |
| Monounsaturated Fatty Acids | Oleic acid (C18:1) | Olive oil Avocados | Energy storage Membrane fluidity modulation | Metabolic syndrome |
 A summary of synthesis and metabolic pathways for both ω‐3 and ω‐6 PUFAs (Cinquina V et al., 2023)
A summary of synthesis and metabolic pathways for both ω‐3 and ω‐6 PUFAs (Cinquina V et al., 2023)
More detailed information on long chain fatty acids can be found here "What Are Long-Chain Fatty Acids? A Beginner's Guide".
More detailed analysis strategies for long chain fatty acids can be read "Analytical Strategies for Long-Chain Fatty Acids Profiling".
Services You May Be Interested In:
2 Core Physiological Role in Health Maintenance
2.1 Neurodevelopmental and Cognitive Functions
Long-chain polyunsaturated fatty acids (LC-PUFAs) serve as fundamental structural constituents for neural myelination. Docosahexaenoic acid (DHA) constitutes over 20% of cerebral gray matter lipids and modulates cognitive performance through synaptic plasticity regulation and neurotransmitter dynamics. Clinical evidence demonstrates:
Infant Neurodevelopment
- Breast milk provides an optimal DHA/arachidonic acid (AA) ratio (1:1-2:1), enabling synergistic bioactivity
- Non-supplemented formula feeding reduces brain tissue and erythrocyte membrane DHA by 30-40% versus breastfed infants
- DHA+AA fortified formula elevates erythrocyte ω-3 index by 0.8% and enhances cognitive scores by 7 points (at 18 months) (Giannì ML et al., 2012)
Adult Cognitive Preservation
- Ω-3 PUFAs exhibit dose-dependent neuroprotection in aging populations:
- Daily intake >500 mg (EPA≥420 mg) improves executive function (effect size d=0.35)
- Primary mechanisms: Frontal cortex protection: Combats oxidative stress via synaptic plasticity modulation
- Supplementation protocol:
- Baseline: 300 mg/day (blood DHA+EPA >4%)
- Intensive phase: 500-800 mg/day for ≤12 months (EPA≥60%) for maximal cognitive benefit (Suh SW et al., 2024)
Neuroprotective Signaling
- DHA demonstrates selective enrichment in synaptic membranes (50% composition) and retinal photoreceptors, reflecting specialized roles in excitable tissue function. During cerebral ischemia-reperfusion:
- Phospholipase A2 hydrolyzes membrane phospholipids within seconds, liberating free DHA and AA
- Temporal release profile: DHA peaks 5-15 minutes post-injury
- Metabolic conversion to neuroprotectin D1 (NPD1) establishes dynamic neuroprotective signaling (Bazan NG 2005)
2.2 Cardiovascular Protective Mechanisms
ω-3 long-chain fatty acids preserve cardiovascular homeostasis through three synergistic pathways:
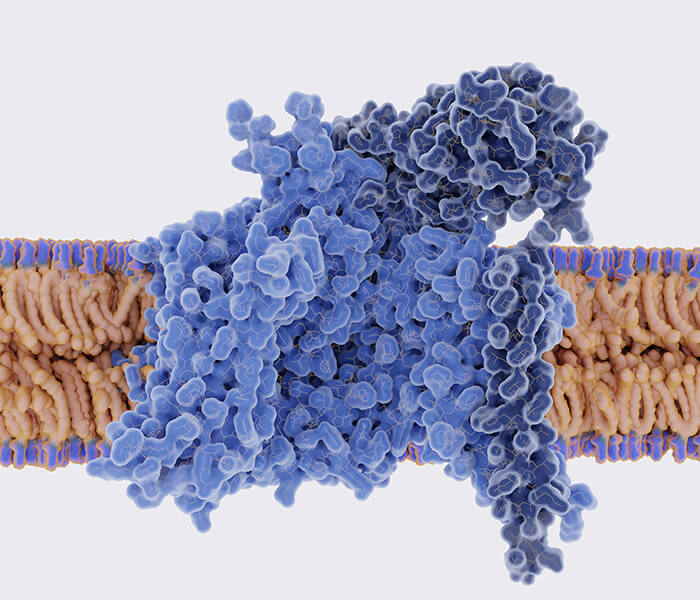
Membrane Receptor Modulation
- These polyunsaturated fatty acids incorporate into phospholipid bilayers, altering membrane architecture to regulate:
- Lipid spatial organization
- Aqueous permeability
- Receptor signaling dynamics
- Computational simulations demonstrate significant enhancement of membrane fluidity, providing mechanistic insight into their cardioprotective and anti-inflammatory actions (Ayee MAA et al., 2020)
Metabolic Coordination
- ω-3 compounds (particularly ALA and DHA) potentiate exercise-induced inflammation reduction:
- Each 10 mL/kg/min VO₂max increase reduces CRP by 32% with adequate ω-3 status
- This synergistic anti-inflammatory interaction is most pronounced in males, Caucasian populations, and individuals with BMI<25 kg/m²
- High saturated fat intake diminishes this cooperative effect
Clinical Implication: Combined ω-3 supplementation and physical activity represents an optimized cardiovascular protection strategy (Farley G et al., 2021)
Hemodynamic Regulation
| Intervention Context | Key Findings | Clinical Evidence |
|---|---|---|
| Primary Prevention | General population benefits require targeted implementation: - Low-dose supplementation (<1g/day) shows limited efficacy (VITAL trial) - Significant risk reduction only in high-risk subgroups:
| Population-based cohort studies |
| Secondary Prevention | High-purity EPA ethyl ester (1.8g/day) achieves: - 25% reduction in major adverse cardiovascular events (REDUCE-IT trial) - Optimal outcomes when initiated ≤30 days post-MI with ≥6 months duration | Randomized controlled trials |
| Dietary Exposure | EPA+DHA intake (per 1g/day increment): - 10% lower coronary heart disease risk (RR 0.90, 95%CI 0.85-0.96) - 12% reduced sudden cardiac death - Maximal benefit with ≥2 fatty fish servings/week | Prospective cohort data |
Core Conclusion: ω-3 LCFAs exhibit dose-dependent cardioprotection with population-specific efficacy thresholds (Innes JK et al.,2020)
2.3 Immunomodulation and Inflammatory Control
Long-chain fatty acids function as immunometabolic regulators through three principal mechanisms:
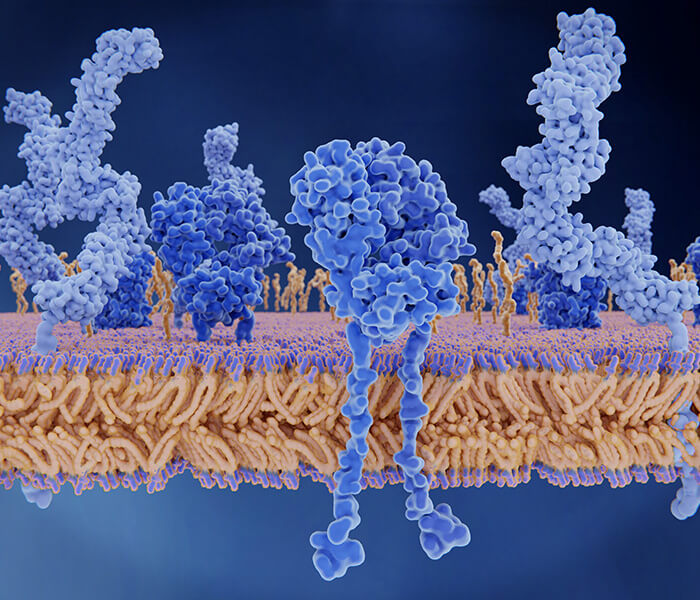
Membrane Biophysical Modulation
Docosahexaenoic acid (DHA) enhances T lymphocyte membrane fluidity, facilitating immune synapse assembly and improving antigen-presenting cell efficiency by 20-35%.
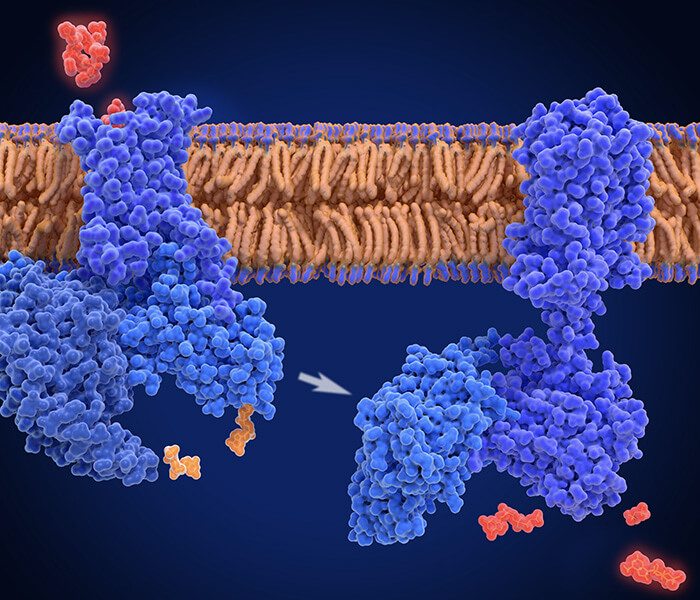
Receptor-Mediated Immunoregulation
- ω-3 PUFAs exhibit dual-mode T-cell regulation:
- Indirect pathway: Modulates antigen-presenting cell (APC) function to influence T-cell activation
- Direct pathway: Governs T-cell subset differentiation and functionality
- Key findings:
- ↑ Regulatory T cells (Tregs) and Th22 populations (up to 40% increase in colitis models)
- ↓ Pro-inflammatory Th1/Th2/Th17 lineages
- Note: Peripheral blood T-cell distribution remains unchanged under homeostasis, demonstrating context-dependent immunomodulation (Gutiérrez S et al.,2019)
Differential Anti-inflammatory Actions
EPA and DHA exert distinct immunomodulatory effects despite shared anti-inflammatory properties:
| Parameter | EPA Effects | DHA Effects |
|---|---|---|
| Leukocyte function | Modulates phagocytosis kinetics | Alters chemotactic responses |
| Genetic regulation | Unique lymphocyte transcriptome profiles | Differential signaling pathway activation |
| Cytotoxicity | Dose-dependent β-cell toxicity | Regulates apoptosis-related proteins (Gorjão R et al., 2009) |
Clinical Translation Evidence
Psoriasis management studies reveal:
| Intervention | Monotherapy Outcomes | Combination Therapy Efficacy |
|---|---|---|
| PASI score | No significant improvement | Mean reduction: -3.92 (95%CI: -6.15 to -1.69) |
| Lesion area | No change (P>0.05) | Mean decrease: -30.00% (95%CI: -33.82 to -26.18) |
| Pruritus symptoms | Unaltered | Synergistic relief observed |
Safety profile: Excellent tolerability in combination regimens (Chen X et al., 2020)
3. Pathological Dualities in Disease Pathogenesis
3.1 Metabolic Dysregulation and Energetic Failure
Inherited or acquired defects in long-chain fatty acid (LCFA) catabolic pathways precipitate systemic energy deficits and toxic metabolite accumulation:
LCHAD Deficiency Pathology
- Accumulation of long-chain 3-hydroxyacylcarnitines in cardiac tissue
- Clinical manifestations:
- Sudden infant death (3-5% of neonatal mortality)
- Dilated cardiomyopathy (LVEF<30%)
Placental Metabolic Dysfunction
- Inverse correlation: LCHAD activity vs. gestational age (r = -0.73)
- Pathological cascade:
- Defective fatty acid oxidation → unmetabolized LCFA entry into maternal circulation
- HELLP syndrome incidence ↑ 8-fold
- Acute gestational fatty liver development
Progressive sequelae:
- Phase I: Neonatal hepatic dysfunction (Reye-like syndrome), hypoketotic hypoglycemia, myopathy
- Phase II: Peripheral neuropathy, retinopathy (Hayes B et al., 2007)
Mitochondrial Homeostatic Failure
| Pathogenic Mechanism | Biochemical Consequence | Disease Linkage |
|---|---|---|
| ACSL overactivation (Regulator of C12-C22 FA flux) | Redirects LCFAs toward membrane biogenesis vs. β-oxidation | Diabetic pathophysiology |
| LCFA mitochondrial overload | ↑ ROS production by 300% | Pancreatic β-cell insulin secretory failure (Rossi Sebastiano M et al., 2019) |
3.2 Neurodegenerative Pathologies
Dysregulation of very long-chain fatty acid (VLCFA) metabolism demonstrates significant associations with multiple neurological disorders:
Glial-Neuronal Axis Dysfunction
VLCFAs accumulating during demyelination or aging undergo glial conversion to sphingosine-1-phosphate (S1P), activating NF-κB signaling cascades that drive neuroinflammation and macrophage infiltration. Therapeutic intervention in multiple sclerosis (MS) mouse models reveals:
- Combined VLCFA inhibitor (bezafibrate) and S1P receptor antagonist (fingolimod) administration achieves synergistic symptom alleviation
- Establishes VLCFA-S1P axis targeting as novel strategy for demyelinating conditions (Chung HL et al., 2023)
Ischemic Neuroprotection
Cerebral ischemia models demonstrate linalool efficacy (25 mg/kg/day oral):
| Functional Domain | Observed Improvement | Biochemical Correlates |
|---|---|---|
| Motor/Cognitive | Significant recovery | ↓ Hippocampal neuroinflammation (astrogliosis/microglial activation) |
| Phospholipid homeostasis | Profile normalization | Restored PC 36:1 and LPC 22:6 concentrations |
| Cellular integrity | Enhanced preservation | Maintained ATP levels + ↓ LDH release (>50% reduction) |
Mechanistic insight: Neurological recovery mediated through phospholipid stabilization (Sabogal-Guáqueta AM et al., 2018)
Blood-Brain Barrier Preservation
Omega-3 intervention in rotenone-induced Alzheimer's models:
| Parameter | Omega-3 Effect | Magnitude |
|---|---|---|
| Oxidative stress | ↓ Lipid peroxidation & ROS | 40-60% reduction |
| Antioxidant capacity | ↑ Catalase/GPx/SOD activity | 2-3 fold enhancement |
| Cellular viability | ↓ Apoptotic rate | >50% reduction (flow cytometry) |
Therapeutic implication: Augments endothelial antioxidant defenses to delay AD progression (Wang L et al., 2018)
3.3 Oncogenic Metabolic Reprogramming
Malignant cells co-opt long-chain fatty acid metabolism to fuel neoplastic progression through three distinct pathways:
Anabolic Rewiring
Long-chain acyl-CoA synthetases (ACSLs) demonstrate subtype-specific roles in breast cancer:
| Isoform | Expression Pattern | Functional Consequence | Clinical Relevance |
|---|---|---|---|
| ACSL1 | Upregulated across subtypes | Enhanced lipid anabolism | Correlates with poor prognosis |
| ACSL3 | Suppressed by CDCP1 in TNBC | ↑ Fatty acid oxidation (FAO) | Promotes metastasis |
| ACSL4 | Elevated in resistant tumors | Activates ABC transporters | Mediates chemotherapy resistance |
| ACSL5 | Hormone receptor-associated | Unknown mechanism | Potential diagnostic marker (Rossi Sebastiano M et al., 2019) |
Ferroptotic Vulnerability Modulation
ACSL4 exhibits context-dependent oncogenic functions:
- Pro-tumorigenic: Facilitates castration-resistant transformation
- Therapeutic vulnerability: Enhances cancer cell sensitivity to ferroptosis by:
- Integrating polyunsaturated fatty acids into phospholipids (phosphatidylethanolamine/phosphatidylinositol)
- Creating peroxidation-susceptible membrane domains
- Clinical implication: Ferroptosis induction represents novel strategy against ACSL4+ malignancies (basal-like breast/colorectal cancers) (Rossi Sebastiano M et al., 2019)
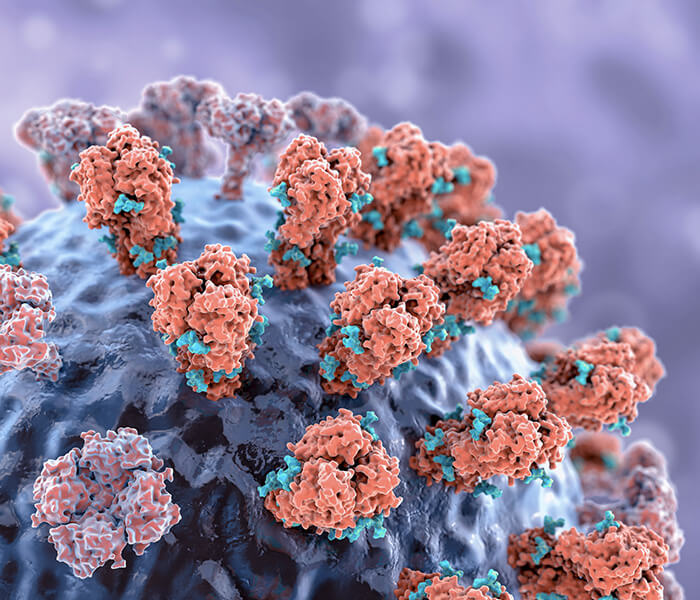
Immunometabolic Escape
Research demonstrates that ketogenic dietary regimens elevate stearic acid (C18:0) levels through gut microbiota modulation, exerting dual anticancer activity against colorectal malignancies:
- Direct Tumor Suppression
- Stearic acid selectively activates PPARα/γ signaling pathways
- Triggers cancer-specific apoptosis (distinct from oleic acid/C18:1 ineffectiveness)
- Indirect Immunoregulation
- Inhibits CD4⁺ T-cell differentiation into Th17 lineage
- Attenuates pro-inflammatory cytokine production (IL-17↓ >60%)
- Creates anti-tumorigenic microenvironment
- Key insights:
- Stearic acid (not SCFAs) mediates primary ketogenic antitumor effects
- Optimal dietary sources: Cocoa butter (40-50% C18:0), animal fats (e.g., butter 30% C18:0)
- Oleic acid (C18:1) lacks comparable efficacy (Tsenkova M et al., 2025)
 The microbial metabolite stearate exhibits anti-cancer effects (Tsenkova M et al., 2025)
The microbial metabolite stearate exhibits anti-cancer effects (Tsenkova M et al., 2025)
4 Intervention strategies based on metabolic regulation
4.1 Nutritional Modulation and Precision Supplementation
Tailoring long-chain fatty acid (LCFA) intake to specific physiological demands:
Neuroprotective Regimen
- Infants/Children: Minimum 100 mg/day docosahexaenoic acid (DHA)
- Cognitive-Impaired Elderly: 1 g/day algal-derived DHA supplementation
→ Achieves 28% elevation in cerebrospinal fluid DHA concentrations (Swanson D et al., 2012)
Cardiovascular Risk Mitigation
- Coronary Artery Disease Patients: Mediterranean diet implementation featuring:
- ω-3-rich seafood
- High-purity olive oil
→ 30% cardiovascular event risk reduction
- Critical parameter: Maintain ω-6/ω-3 ratio<4:1 (Swanson D et al., 2012)
Oncopreventive Ketogenic Protocol
- Colorectal Cancer High-Risk Cohort:
- Prioritize stearic acid sources:
- Cocoa butter (40% C18:0)
- Dairy lipids (e.g., butter: 30% C18:0)
- Synergize with probiotic co-administration (e.g., Bifidobacterium adolescentis)
→ Potentiates antitumor efficacy (Tsenkova M et al., 2025)
- Synergize with probiotic co-administration (e.g., Bifidobacterium adolescentis)
4.2 Therapeutic Target Development
Pharmacological strategies targeting critical long-chain fatty acid (LCFA) metabolic nodes:
ACSL Isoform Modulation
- ACSL3 activation via mTORC1-SREBP signaling promotes treatment resistance in malignancies (e.g., NSCLC, prostate cancer) through:
- Fatty acid oxidation-dependent energy production
- Steroid biosynthesis potentiation
- Therapeutic approaches:
- Combine with FAO inhibitors (etomoxir)
- Synergize with ER stress inducers
- Block androgen synthesis escape in prostate cancer
- Critical consideration: ACSL3 downregulation in TNBC necessitates tumor molecular subtyping prior to intervention (Rossi Sebastiano M et al., 2018)
Stearate-Mediated Oncotherapy
| Mechanism | Experimental Evidence | Clinical Translation |
|---|---|---|
| Stearic acid (SA) |
| Dietary SA enrichment (33%) + CAY10566 → tumor inhibition (p<0.05) |
| Oleic acid (OA) | Antagonizes SA-mediated apoptosis | OA supplementation abrogates SA anticancer effects |
| SCD1 blockade | Prevents SA→OA conversion |
- Novel strategy: Dual modulation of SA/OA ratio through diet and SCD1 inhibition (Jumpei Ogura et ., 2024)
Peroxisomal Pathway Activation
Peroxisome dysfunction (PEX/non-PEX mutations) causes disease spectrum characterized by:
- Defective VLCFA β-oxidation (pathway exclusivity)
- VLCFA accumulation as diagnostic hallmark
- Clinical manifestations:
- Neonatal: Zellweger syndrome (malformations, multi-organ failure)
- Adult-onset: X-linked adrenoleukodystrophy
- → Represents emerging class of rare metabolic disorders (Stradomska TJ 2018)
- Clinical manifestations:
References
- Giannì ML, Roggero P, Baudry C, Ligneul A, Morniroli D, Garbarino F, le Ruyet P, Mosca F. "The influence of a formula supplemented with dairy lipids and plant oils on the erythrocyte membrane omega-3 fatty acid profile in healthy full-term infants: a double-blind randomized controlled trial." BMC Pediatr. 2012 Oct 17;12:164. doi: 10.1186/1471-2431-12-164
- Cinquina V, Keimpema E, Pollak DD, Harkany T. "Adverse effects of gestational ω-3 and ω-6 polyunsaturated fatty acid imbalance on the programming of fetal brain development." J Neuroendocrinol. 2023 Sep;35(9):e13320. doi: 10.1111/jne.13320
- Suh SW, Lim E, Burm SY, Lee H, Bae JB, Han JW, Kim KW. "The influence of n-3 polyunsaturated fatty acids on cognitive function in individuals without dementia: a systematic review and dose-response meta-analysis." BMC Med. 2024 Mar 12;22(1):109. doi: 10.1186/s12916-024-03296-0
- Bazan NG. "Neuroprotectin D1 (NPD1): a DHA-derived mediator that protects brain and retina against cell injury-induced oxidative stress." Brain Pathol. 2005 Apr;15(2):159-66. doi: 10.1111/j.1750-3639.2005.tb00513.x
- Djuricic I, Calder PC. "Pros and Cons of Long-Chain Omega-3 Polyunsaturated Fatty Acids in Cardiovascular Health." Annu Rev Pharmacol Toxicol. 2023 Jan 20;63:383-406. doi: 10.1146/annurev-pharmtox-051921-090208
- Ayee MAA, Bunker BC, De Groot JL. "Membrane modulatory effects of omega-3 fatty acids: Analysis of molecular level interactions." Curr Top Membr. 2020;86:57-81. doi: 10.1016/bs.ctm.2020.08.001
- Farley G, Riggs DW, Bhatnagar A, Hellmann J. "Omega-3 polyunsaturated fatty acids modify the inverse association between systemic inflammation and cardiovascular fitness." Clin Nutr. 2021 Jun;40(6):4097-4105. doi: 10.1016/j.clnu.2021.02.006
- Innes JK, Calder PC. "Marine Omega-3 (N-3) Fatty Acids for Cardiovascular Health: An Update for 2020." Int J Mol Sci. 2020 Feb 18;21(4):1362. doi: 10.3390/ijms21041362
- Gutiérrez S, Svahn SL, Johansson ME. "Effects of Omega-3 Fatty Acids on Immune Cells." Int J Mol Sci. 2019 Oct 11;20(20):5028. doi: 10.3390/ijms20205028
- Gorjão R, Azevedo-Martins AK, Rodrigues HG, Abdulkader F, Arcisio-Miranda M, Procopio J, Curi R. "Comparative effects of DHA and EPA on cell function." Pharmacol Ther. 2009 Apr;122(1):56-64. doi: 10.1016/j.pharmthera.2009.01.004
- Chen X, Hong S, Sun X, Xu W, Li H, Ma T, Zheng Q, Zhao H, Zhou Y, Qiang Y, Li B, Li X. "Efficacy of fish oil and its components in the management of psoriasis: a systematic review of 18 randomized controlled trials." Nutr Rev. 2020 Oct 1;78(10):827-840. doi: 10.1093/nutrit/nuz098
- Hayes B, Lynch B, O'Keefe M, Monavari AA, Treacy EP. "Long chain fatty acid oxidation defects in children: importance of detection and treatment options." Ir J Med Sci. 2007 Sep;176(3):189-92. doi: 10.1007/s11845-007-0025-y
- Rossi Sebastiano M, Konstantinidou G. "Targeting Long Chain Acyl-CoA Synthetases for Cancer Therapy." Int J Mol Sci. 2019 Jul 24;20(15):3624. doi: 10.3390/ijms20153624
- Chung HL, Ye Q, Park YJ, Zuo Z, Mok JW, Kanca O, Tattikota SG, Lu S, Perrimon N, Lee HK, Bellen HJ. "Very-long-chain fatty acids induce glial-derived sphingosine-1-phosphate synthesis, secretion, and neuroinflammation." Cell Metab. 2023 May 2;35(5):855-874.e5. doi: 10.1016/j.cmet.2023.03.022
- Sabogal-Guáqueta AM, Posada-Duque R, Cortes NC, Arias-Londoño JD, Cardona-Gómez GP. "Changes in the hippocampal and peripheral phospholipid profiles are associated with neurodegeneration hallmarks in a long-term global cerebral ischemia model: Attenuation by Linalool." Neuropharmacology. 2018 Jun;135:555-571. doi: 10.1016/j.neuropharm.2018.04.015
- Wang L, Fan H, He J, Wang L, Tian Z, Wang C. "Protective effects of omega-3 fatty acids against Alzheimer's disease in rat brain endothelial cells." Brain Behav. 2018 Nov;8(11):e01037. doi: 10.1002/brb3.1037
- Tsenkova M, Brauer M, Pozdeev VI, Kasakin M, Busi SB, Schmoetten M, Cheung D, Meyers M, Rodriguez F, Gaigneaux A, Koncina E, Gilson C, Schlicker L, Herebian D, Schmitz M, de Nies L, Mayatepek E, Haan S, de Beaufort C, Cramer T, Meiser J, Linster CL, Wilmes P, Letellier E. "Ketogenic diet suppresses colorectal cancer through the gut microbiome long chain fatty acid stearate." Nat Commun. 2025 Feb 20;16(1):1792. doi: 10.1038/s41467-025-56678-0
- Swanson D, Block R, Mousa SA. "Omega-3 fatty acids EPA and DHA: health benefits throughout life." Adv Nutr. 2012 Jan;3(1):1-7. doi: 10.3945/an.111.000893
- Jumpei Ogura; Koji Yamanoi; Mana Taki; Ryusuke Murakami; Ken Yamaguchi; Junzo Hamanishi; Masaki Mandai. "Elucidating the influence of long-chain fatty acids on ovarian cancer progression." Other Topics. 2024 Mar;4. doi: 10.1158/1538-7445.OVARIAN23-B107
- Stradomska TJ. "Choroby peroksysomalne [Peroxisomal disorders]." Postepy Biochem. 2018 Dec 29;64(4):359-367. doi: 10.18388/pb.2018_150