Long-chain fatty acids (LCFAs; C12-C22) serve as fundamental components of human energy metabolism and perform critical structural and regulatory functions. They are indispensable for maintaining cellular membrane integrity, modulating signal transduction pathways, and supplying metabolic energy. Impairments within LCFA metabolic pathways trigger complex, multi-system pathologies affecting cardiac, hepatic, muscular, and neurological systems. These disorders arise from either genetic defects (e.g., very long-chain acyl-CoA dehydrogenase deficiency, VLCADD) or acquired conditions (e.g., lipotoxicity associated with metabolic syndrome), exhibiting profound clinical heterogeneity from neonatal mortality to adult-onset neurodegeneration.
Conventional diagnostic approaches face significant limitations. Standard biochemical markers like creatine kinase and transaminases lack specificity, while acute-phase metabolic fluctuations can yield false-negative results.
Metabolomics offers a transformative solution by enabling systematic profiling of dynamic small-molecule metabolite alterations. This technology comprehensively maps metabolic pathway perturbations and identifies highly sensitive and specific biomarkers, providing a robust scientific foundation for early detection, disease subtyping, therapeutic guidance, and prognostic assessment.
Recent advances demonstrate the power of integrated multi-omics strategies. Combining lipidomic, genomic, and proteomic data is progressively elucidating the molecular network dysregulations underlying LCFA disorders. Groundbreaking research revealed how very-long-chain fatty acids (VLCFAs) initiate neuroinflammatory cascades by inducing glial sphingosine-1-phosphate (S1P) synthesis. Furthermore, clinical studies have validated the utility of combinatorial biomarkers for guiding personalized therapeutic interventions.
1. Metabolomics Technologies: Platform Advancements to Data Integration
1.1 Mass Spectrometry Platform Innovations
Contemporary metabolomics leverages high-resolution mass spectrometry coupled with diverse ionization and separation techniques for comprehensive metabolite profiling in complex biological matrices:
- Liquid Chromatography-Mass Spectrometry (LC-MS): High-resolution platforms—particularly ultra-high performance liquid chromatography (UHPLC) systems like the Shimadzu Nexera LC-30A paired with Q-Exactive Plus mass spectrometers—enable exceptional lipid structural resolution. Employing an ACQUITY UPLC CSH C18 column (1.7 μm, 2.1 × 100 mm) with a binary gradient elution system (Mobile Phase A: 0.1% formic acid/0.1 mM ammonium formate in acetonitrile-water; Mobile Phase B: 0.1% formic acid/0.1 mM ammonium formate in acetonitrile-isopropanol) achieves baseline separation of phospholipid isomers at 70,000 resolution (m/z 200). This capability proved critical in neurodegeneration research, identifying neurotoxic phospholipids like PC(20:3:6) associated with VLCFA pathology.
- Gas Chromatography-Mass Spectrometry (GC-MS): This platform excels in fatty acid quantification, especially for short-to-medium chain species (C8-C30). Derivatization enables detection at 0.1 amu resolution. Its integration with tandem MS (MS/MS) in newborn screening allows simultaneous acylcarnitine profiling, achieving >90% diagnostic sensitivity for VLCADD. Elevated myristenylcarnitine (C14:1 >1 μmol/L) provides specific diagnostic evidence, even pre-symptomatically.
- Imaging Mass Spectrometry: Spatial metabolomics advances through techniques like MALDI-MSI (Matrix-Assisted Laser Desorption/Ionization Mass Spectrometry Imaging) permit in situ tissue metabolite mapping. This revealed pathological S1P enrichment within demyelinating lesions on brain sections, offering unique insights into metabolic tissue heterogeneity.
 Liquid Chromatography Triple Quadrupole Mass Spectrometry Multiple Reaction Monitoring targeted metabolomics experiment (Roberts LD et al., 2012)
Liquid Chromatography Triple Quadrupole Mass Spectrometry Multiple Reaction Monitoring targeted metabolomics experiment (Roberts LD et al., 2012)
For more information on long-chain fatty acid analysis strategies, please refer to "Analytical Strategies for Long-Chain Fatty Acids Profiling".
1.2 Bioinformatics and Multi-Omics Integration
Advanced computational tools are essential for interpreting complex metabolomic datasets:
- Metabolic Pathway Analysis: Platforms (MetaboAnalyst, Mummichog) identify dysregulated pathways. In VLCADD, S1P pathway activation correlates with neuroinflammation. Drosophila models confirm this: glial-specific ELOVL1 overexpression elevates VL-ceramide and S1P, directly linking sphingolipid dysmetabolism to motor deficits.
- Machine Learning-Driven Biomarker Discovery: Algorithms (Random Forest, Support Vector Machines) process high-dimensional data to identify diagnostic signatures. For mild cognitive impairment (MCI), a machine learning-derived panel (cholinesterase activity, C24:0/C22:0 ratio, C22:6, L-Glutamine) achieved 89% diagnostic accuracy.
- Multi-Omics Data Integration:
- Epigenetic-Metabolic Crosstalk: Combined ChIP-seq/metabolomics revealed PPARγ CpG island hypomethylation (10% reduction) associates with significant weight loss (2.1 kg, p=0.003).
- Cell-Type Specific Pathology: Integrating single-cell RNA-seq with lipidomics identified oligodendrocyte-specific ACOX1 downregulation as a key driver of VLCFA accumulation in white matter.
2. Discovery and Validation of Disease-Specific Biomarkers
2.1 Inborn Errors of Metabolism: Screening to Precision Subtyping
Early detection of cardiometabolic disorders is critical for mortality reduction. As the most prevalent long-chain fatty acid oxidation defect, VLCADD newborn screening utilizes tandem mass spectrometry (MS/MS) to profile acylcarnitines in dried blood spots:
- C14:1 Acylcarnitine: Significantly elevated (>1 μmol/L) in cardiomyopathy-type VLCADD, correlating with myocardial lipid deposition severity. Notably, ~15% of asymptomatic patients yield false negatives, necessitating confirmatory genetic testing.
- C14:1/C2 Ratio: Superior specificity to single markers, differentiating true positives from false positives. A ratio >0.02 yields a positive likelihood ratio of 18.5 for VLCADD diagnosis.
- C14:1/C16 Ratio: Demonstrates enhanced diagnostic value in hepatic-type VLCADD, with abnormal elevation preceding conventional liver function abnormalities.
Table: Characteristic Biomarkers in Fatty Acid Metabolism Disorders
| Disorder Type | Key Biomarkers | Sample | Technology | Clinical Manifestations |
|---|---|---|---|---|
| VLCADD (Cardiomyopathy) | C14:1 ↑↑, C14:1/C2 ↑ | Dried blood spots, Plasma | MS/MS | Hypertrophic cardiomyopathy, Arrhythmia |
| VLCADD (Hepatic) | Dicarboxylic acids (C6-C14) ↑, C14:1/C16 ↑ | Urine, Plasma | GC-MS | Hypoketotic hypoglycemia, Hepatomegaly |
| Neurodegenerative Disease | S1P ↑↑, PC(20:3:6) ↓ | CSF, Brain tissue | LC-MS/MS | Cognitive decline, Motor deficits |
| Tumor Chemoresistance | EPA/DHA ratio ↓, LPC(22:6) ↑ | Serum, Tissue | UHPLC-QE | Reduced chemotherapy sensitivity |
2.2 Neurodegenerative Disease Mechanisms: VLCFA Neurotoxicity
Cerebrospinal fluid (CSF) metabolomics reveals novel VLCFA-mediated neurotoxicity via the VLCFA → VL-Ceramide → S1P pathogenic axis:
- S1P Elevation: CSF S1P concentrations increase 2.3-fold in EAE mice versus controls, strongly correlating with clinical severity (R=0.78).
- Spatiotemporal Dysregulation: Immunofluorescence confirms abnormal neuronal S1P accumulation, triggering mitochondrial apoptosis. Mechanistically, S1P upregulates the phagocytic receptor Draper, promoting glial-mediated neuronal engulfment.
- Phospholipid Alterations: CSF levels of DHA-containing phospholipids (e.g., PC(20:3:6), LPC(22:6)) are significantly reduced, indicating membrane instability. These changes precede cognitive test abnormalities in mild cognitive impairment (MCI) patients (Chung HL et al., 2023).
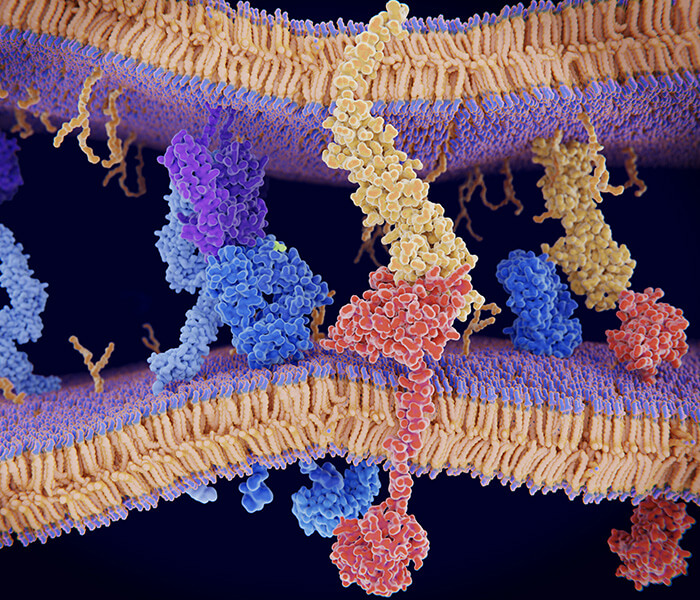
 Elevated S1P induces phagocytosis through Draper (Chung HL et al., 2023)
Elevated S1P induces phagocytosis through Draper (Chung HL et al., 2023)
The use of long-chain fatty acids in neurological diseases can be read "Case Study: Metabolomic Profiling of Very Long-Chain Fatty Acids in Neurological Disease".
2.3 Acquired Metabolic Disorders: From Hepatic Steatosis to Oncogenic Remodeling
Metabolomic Signatures in NAFLD/NASH: Lipidomic profiling of nonalcoholic fatty liver disease (NAFLD) patients reveals profound reprogramming. Key alterations in plasma include:
- Systemic Lipid Imbalance: A decreased phosphatidylcholine (PC) to triglyceride (TG) ratio alongside elevated lysophosphatidylethanolamine (LPE) levels, indicative of impaired hepatocyte membrane synthesis capacity (Guo X et al., 2022).
- NASH-Specific Biomarkers: Phosphatidylinositol (PI(36:2)) and specific diglyceride (DG) species containing palmitoleic acid (C16:1) are significantly elevated in nonalcoholic steatohepatitis (NASH). These markers show a positive correlation with liver fibrosis severity (AUROC = 0.82) (Xu X et al., 2022).
Metabolic Remodeling in the Tumor Microenvironment and Therapeutic Implications: Metabolic adaptations within tumors significantly influence treatment efficacy. Omega-3 long-chain polyunsaturated fatty acids (LC-PUFAs), notably eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), enhance chemotherapy response through multiple mechanisms:
- Modulation of Membrane Properties: DHA incorporates into tumor cell membranes, increasing fluidity and facilitating intracellular uptake of chemotherapeutic agents. For example, in HER2-positive breast cancer, a unit increase in the EPA/DHA ratio correlated with a 2.7-fold rise in intracellular doxorubicin concentration.
- Induction of Apoptosis: Resolvin D1, a metabolite of DHA, potentiates TRAIL-induced apoptosis by suppressing the NF-κB pathway. Clinically, omega-3 PUFA supplementation increased oxaliplatin response rates by 35% in metastatic colorectal cancer patients.
- Biomarkers of Chemoresistance: Lysophosphatidylcholine (LPC(22:6)) levels demonstrate a significant inverse correlation (r = -0.63) with Multidrug Resistance Protein 1 (MDR1) expression, suggesting its potential as a biomarker for predicting chemotherapy sensitivity (Fodil M et al., 2022).
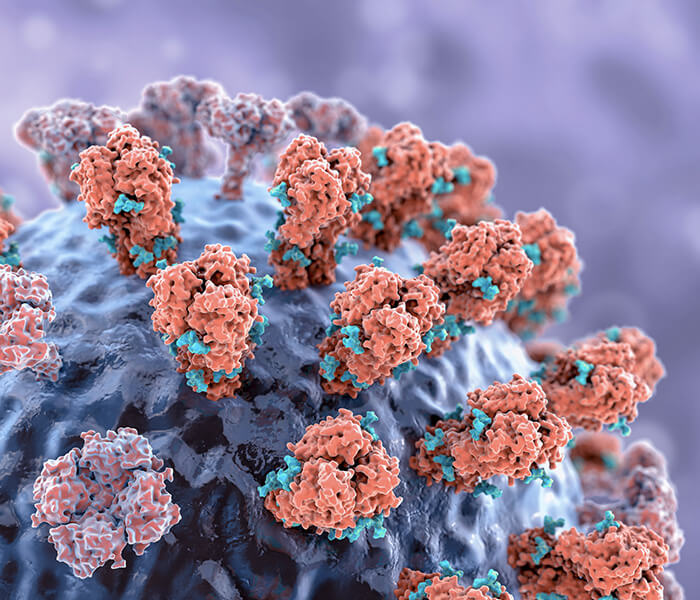
 Anti-inflammatory effects of n-3 LC-PUFAs related to obesity and breast cancer (Fodil M et al., 2022)
Anti-inflammatory effects of n-3 LC-PUFAs related to obesity and breast cancer (Fodil M et al., 2022)
Services You May Be Interested In:
3. Metabolomics-Driven Precision Medicine
3.1 Transforming Diagnostic and Classification Paradigms
Metabolomics is fundamentally redefining the diagnosis and subtyping of long-chain fatty acid oxidation disorders (LC-FAODs):
- Revolutionizing Newborn Screening:
- Traditional screening, reliant on single acylcarnitine markers, suffers from high false-positive rates (~40%).
- Implementing multivariate diagnostic models incorporating indices like C14:1, C14:1/C2, and C14:1/C16 significantly boosts positive predictive value (PPV) from 25% to 92%.
- Screening for ACADVL (Very Long-Chain Acyl-CoA Dehydrogenase) gene carriers identified a diagnostic gray zone (C14:1 levels 0.8-1.0 μmol/L), necessitating confirmation via exon sequencing (Tajima G et al., 2024).
- Cerebrospinal Fluid (CSF) Metabolic Subtyping in Neurodegeneration:
- CSF metabolomics enables precise disease classification, forming the foundation for targeted therapies.
- Multiple sclerosis (MS) exemplifies this, stratifying into three distinct metabolic subtypes:
- Sphingosine-1-phosphate (S1P) dominant (45%)
- Mitochondrial dysfunction (30%)
- Mixed (25%)
- Therapeutic response varies significantly by subtype: S1P-dominant patients exhibit high fingolimod response rates (85%), while the mitochondrial dysfunction subtype shows better outcomes with coenzyme Q10 combined with medium-chain triglycerides (MCT) (Kwon EH et al., 2022).
- Dynamic Metabolic Pathway Assessment via Stable Isotopes:
- Stable isotope tracers facilitate real-time quantification of metabolic flux dynamics.
- Experiments utilizing ¹³C₃-glycerol, with or without heptanoate (C7, the active component of triheptanoin), quantified hepatic gluconeogenic flux.
- Key Findings in VLCAD-/- Mice:
- The significant difference in ¹³C₃-glycerol incorporation into blood glucose between VLCAD-/- and wild-type (WT) mice disappeared following C7 administration.
- C7 significantly reduced ¹³C enrichment in liver metabolites of VLCAD-/- mice.
- Interpretation: C7 efficiently supplies alternative gluconeogenic precursors (C5 ketone bodies), meeting the elevated substrate demand in VLCAD deficiency and reducing reliance on glycerol (Nurjanah S et al., 2023).
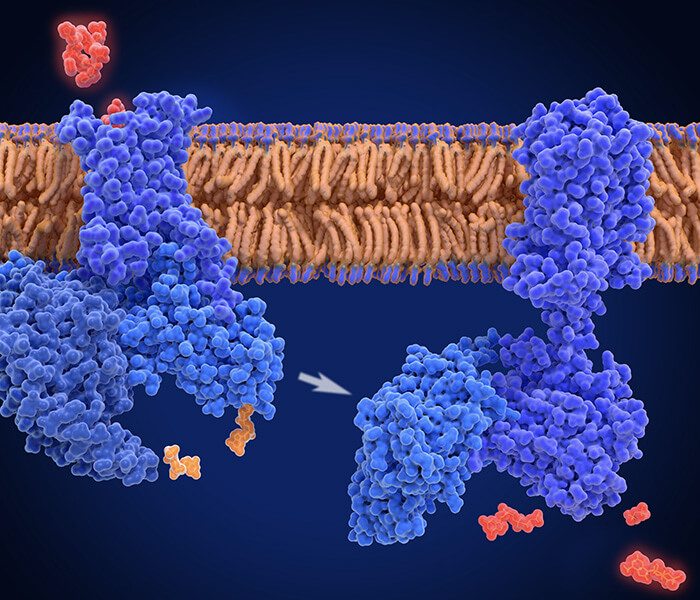
 Blood measurement in VLCAD−/− mice with heptanoate (C7) (Nurjanah S et al., 2023)
Blood measurement in VLCAD−/− mice with heptanoate (C7) (Nurjanah S et al., 2023)
3.2 Innovations in Targeted Intervention Strategies
Metabolomic biomarkers now enable highly individualized therapeutic approaches, moving beyond traditional one-size-fits-all paradigms:
- Precision Nutrition Intervention:
- Conventional medium-chain triglyceride (MCT) supplementation strategies lack personalization.
- A phase I clinical trial evaluated Lipistat™, a novel high-MCT (30%) formula specifically designed for pediatric long-chain fatty acid β-oxidation disorders (LCFAOD).
- This 6-7 day study demonstrated promising safety and tolerability in 6 enrolled children (5 completed), with no significant adverse events or associated symptoms reported (MacDonald A et al., 2018).
- Drug Repositioning Based on Mechanism:
- Fingolimod, an S1P receptor modulator, exhibits dual activity in experimental autoimmune encephalomyelitis (EAE) models: inhibiting S1P receptor-mediated lymphocyte migration and reducing neuronal S1P accumulation.
- Combining fingolimod with the peroxisome proliferator-activated receptor (PPAR) agonist bezafibrate yielded an 82% improvement in clinical scores, substantially outperforming monotherapy efficacy (45-50%) (Chung HL et al., 2023).
- Gene Therapy Targeting with Biomarker Monitoring:
- Clinical trials employing AAV9 vectors for ACADVL gene therapy successfully normalized patient acylcarnitine profiles.
- A critical consideration emerged: during metabolic stress (when >60% energy derives from fat), vector expression may inadequately compensate, highlighting the need for careful monitoring under high-fat metabolic demand (Keeler AM et al., 2012).
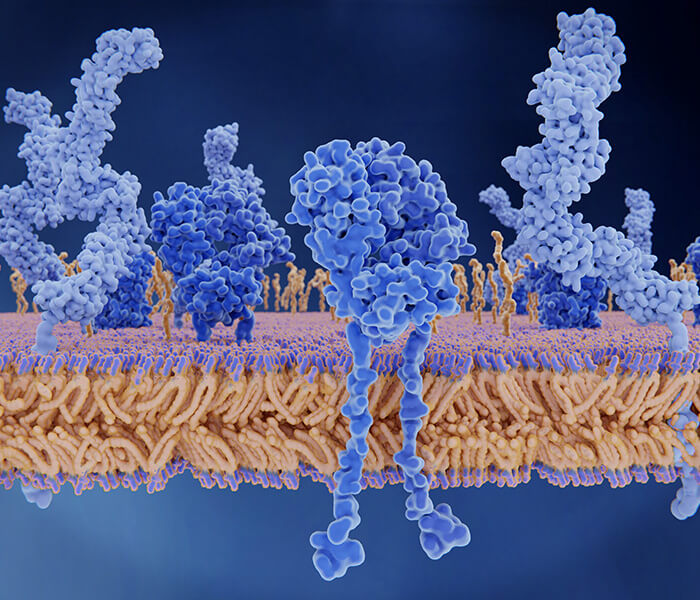
 Transduction and expression of rAAV9-VLCAD (Keeler AM et al., 2012)
Transduction and expression of rAAV9-VLCAD (Keeler AM et al., 2012)
- Table: Biomarker-Guided Precision Intervention Strategies
| Biomarker | Intervention Strategy | Mechanism of Action | Clinical Evidence |
|---|---|---|---|
| Plasma C14:1 > 1 μmol/L | MCT Replacement (20% total calories) | Bypasses VLCAD deficiency | Cardiomyopathy subtype 1-year survival increased from 60% to 92% |
| CSF S1P ↑ | Fingolimod + Bezafibrate | Inhibits S1P synthesis & signaling | EAE model clinical scores improved by 82% vs. monotherapy (45-50%) |
| Tumor Tissue EPA/DHA < 0.5 | High-Dose ω-3 PUFAs (4 g/day) | Enhances membrane fluidity & pro-apoptotic pathways | Breast cancer chemotherapy response rate increased by 35% |
| Fecal Butyrate < 2 mM | Probiotics (e.g., Akkermansia muciniphila) | Repairs intestinal barrier / Exerts anti-inflammatory effects | NAFLD patients exhibited 40% higher rate of liver enzyme normalization |
4. Challenges and Future Directions
4.1 Technical Bottlenecks and Translation Barriers
- Current metabolomics research confronts significant hurdles:
- Biomarker Validation Gap: Most identified markers remain confined to initial study cohorts, lacking robust multicenter validation. A systematic review of 30 lipid biomarkers revealed only phosphatidylcholine (PC(36:2)) and lysophosphatidylethanolamine (LPE(18:1)) consistently maintained discriminative power (AUROC > 0.8) across independent validation studies.
- Spatial Resolution Limitations: While MALDI mass spectrometry imaging (MALDI-MSI) enables metabolite localization within tissues, it cannot resolve metabolic heterogeneity within subcellular compartments (e.g., mitochondria vs. cytosol). Emerging techniques like nano-scale Secondary Ion Mass Spectrometry (nanoSIMS) with isotopic labeling offer promise, achieving ultra-high spatial resolution (~50 nm) to overcome this barrier.
- Dynamic Monitoring Deficiency: Reliance on static biospecimens (plasma, CSF) represents a major constraint. Developing real-time in vivo metabolic imaging is critical. Fluorinated fatty acid analogue PET probes (e.g., ¹⁸F-FTHA) successfully quantify myocardial fatty acid uptake in vivo but exhibit insufficient blood-brain barrier penetration for neural tissue applications.
4.2 Emerging Frontiers and Clinical Integration
- Interdisciplinary innovation drives future progress:
- Spatial Multi-Omics Convergence: Integrating single-cell transcriptomics with spatial metabolomics has mapped very-long-chain fatty acid (VLCFA) metabolism across brain cell types. Key findings include high expression of elongase ELOVL1 and fatty acid synthase (FASN) in oligodendrocytes, and enrichment of sphingosine kinase 1 (Sphk1, S1P synthase) in microglia, elucidating the specific vulnerability of myelinated areas to VLCFA toxicity.
- Host-Microbiota Metabolic Crosstalk: Gut microbiota metabolize long-chain fatty acids (LCFAs) into odd-chain fatty acids (e.g., pentadecanoic acid C15:0, heptadecanoic acid C17:0) with signaling functions. Akkermansia muciniphila abundance correlates strongly with metabolic health; each 1 log-unit increase associates with a 30% improvement in insulin sensitivity, mediated partly by C15:0 activation of peroxisome proliferator-activated receptor gamma (PPARγ).
- Minimally Invasive Biosensing: Neuron-derived exosomes overcome the blood-brain barrier, enabling liquid biopsy for CNS lipid metabolism assessment. Exosomal microRNAs (e.g., miR-122-5p, miR-34a) reflecting brain lipid metabolic states exhibit superior stability compared to free circulating RNA.
- AI-Driven Personalization: Deep learning models integrating multi-omics data predict individual metabolic phenotypes. "Digital twin" systems, for instance, simulate the impact of dietary interventions on acylcarnitine profiles, guiding personalized nutritional support for VLCAD deficiency (VLCADD) patients.
5. Conclusion
Through the deep integration of metabolomics with bioinformatics, we are poised to comprehensively map LC-FAOD pathophysiology at the molecular level, yielding unprecedented mechanistic insights. This convergence promises to ultimately shift the medical paradigm from reactive disease treatment to proactive health maintenance. Realizing this vision demands sustained technological innovation and robust interdisciplinary collaboration among clinicians, metabolic specialists, and biochemists to drive the advancement of precision metabolic medicine.
References
- Roberts LD, Souza AL, Gerszten RE, Clish CB. "Targeted metabolomics." Curr Protoc Mol Biol. 2012 Apr;Chapter 30:Unit 30.2.1-24. doi: 10.1002/0471142727.mb3002s98
- Browning MF, Larson C, Strauss A, Marsden DL. "Normal acylcarnitine levels during confirmation of abnormal newborn screening in long-chain fatty acid oxidation defects." J Inherit Metab Dis. 2005;28(4):545-50. doi: 10.1007/s10545-005-0545-4
- Chung HL, Ye Q, Park YJ, Zuo Z, Mok JW, Kanca O, Tattikota SG, Lu S, Perrimon N, Lee HK, Bellen HJ. "Very-long-chain fatty acids induce glial-derived sphingosine-1-phosphate synthesis, secretion, and neuroinflammation." Cell Metab. 2023 May 2;35(5):855-874.e5. doi: 10.1016/j.cmet.2023.03.022
- Hayes B, Lynch B, O'Keefe M, Monavari AA, Treacy EP. "Long chain fatty acid oxidation defects in children: importance of detection and treatment options." Ir J Med Sci. 2007 Sep;176(3):189-92. doi: 10.1007/s11845-007-0025-y
- Guo X, Yin X, Liu Z, Wang J. "Non-Alcoholic Fatty Liver Disease (NAFLD) Pathogenesis and Natural Products for Prevention and Treatment." Int J Mol Sci. 2022 Dec 7;23(24):15489. doi: 10.3390/ijms232415489
- Xu X, Poulsen KL, Wu L, Liu S, Miyata T, Song Q, Wei Q, Zhao C, Lin C, Yang J. "Targeted therapeutics and novel signaling pathways in non-alcohol-associated fatty liver/steatohepatitis (NAFL/NASH)." Signal Transduct Target Ther. 2022 Aug 13;7(1):287. doi: 10.1038/s41392-022-01119-3
- Fodil M, Blanckaert V, Ulmann L, Mimouni V, Chénais B. "Contribution of n-3 Long-Chain Polyunsaturated Fatty Acids to the Prevention of Breast Cancer Risk Factors." Int. J. Environ. Res. Public Health. 2022; 19(13):7936. doi: 10.3390/ijerph19137936
- Tajima G, Aisaki J, Hara K, Tsumura M, Kagawa R, Sakura F, Sasai H, Yuasa M, Shigematsu Y, Okada S. "Using the C14:1/Medium-Chain Acylcarnitine Ratio Instead of C14:1 to Reduce False-Positive Results for Very-Long-Chain Acyl-CoA Dehydrogenase Deficiency in Newborn Screening in Japan." Int J Neonatal Screen. 2024 Feb 20;10(1):15. doi: 10.3390/ijns10010015
- Kwon EH, Tennagels S, Gold R, Gerwert K, Beyer L, Tönges L. "Update on CSF Biomarkers in Parkinson's Disease." Biomolecules. 2022 Feb 18;12(2):329. doi: 10.3390/biom12020329
- Nurjanah S, Gerding A, Vieira-Lara MA, Evers B, Langelaar-Makkinje M, Spiekerkoetter U, Bakker BM, Tucci S. "Heptanoate Improves Compensatory Mechanism of Glucose Homeostasis in Mitochondrial Long-Chain Fatty Acid Oxidation Defect." Nutrients. 2023 Nov 5;15(21):4689. doi: 10.3390/nu15214689
- MacDonald A, Webster R, Whitlock M, Gerrard A, Daly A, Preece MA, Evans S, Ashmore C, Chakrapani A, Vijay S, Santra S. "The safety of Lipistart, a medium-chain triglyceride based formula, in the dietary treatment of long-chain fatty acid disorders: a phase I study." J Pediatr Endocrinol Metab. 2018 Mar 28;31(3):297-304. doi: 10.1515/jpem-2017-0426
- Keeler AM, Conlon T, Walter G, Zeng H, Shaffer SA, Dungtao F, Erger K, Cossette T, Tang Q, Mueller C, Flotte TR. "Long-term correction of very long-chain acyl-coA dehydrogenase deficiency in mice using AAV9 gene therapy. Mol Ther. 2012 Jun;20(6):1131-8. doi: 10.1038/mt.2012.39. Epub 2012 Mar 6." Erratum in: Mol Ther. 2012 Jun;20(6):1287. doi: 10.1038/mt.2012.39