Altered Glucose Metabolism: A Defining Feature of Cancer Cells
Altered energy metabolism is a biochemical fingerprint of cancer cells that represents one of the "hallmarks of cancer". This metabolic phenotype is characterized by preferential dependence on glycolysis (the process of conversion of glucose into pyruvate followed by lactate production) for energy production in an oxygen-independent manner. Although glycolysis is less efficient than oxidative phosphorylation in the net yield of adenosine triphosphate (ATP), cancer cells adapt to this mathematical disadvantage by increased glucose uptake, which in turn facilitates a higher rate of glycolysis. Apart from providing cellular energy, the metabolic intermediates of glycolysis also play a pivotal role in macromolecular biosynthesis, thus conferring a selective advantage to cancer cells under a diminished nutrient supply[1].
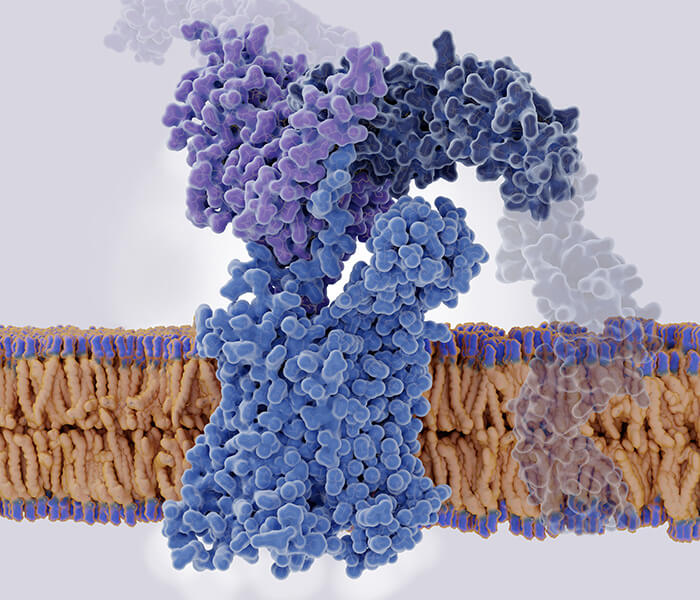
Glucose metabolism in cancer cells is primarily characterized by two major biochemical events: (i) increased glucose uptake and (ii) aerobic glycolysis, the process of conversion of glucose into pyruvate, eventually resulting in the production of lactate (fermentation), fig 1.
 Fig 1. Regulation of glucose metabolism in cancer cells. Glucose metabolism mainly contains glycolysis and the TCA cycle in the mitochondrion. These pathways are generally altered in tumor cells compared to normal cells[2]
Fig 1. Regulation of glucose metabolism in cancer cells. Glucose metabolism mainly contains glycolysis and the TCA cycle in the mitochondrion. These pathways are generally altered in tumor cells compared to normal cells[2]
Key Biochemical Events in Tumor Glycolysis
GLUT Overexpression and Glucose Uptake in Cancer
The most important role of glycolysis is to consume glucose and convert it into energy in the form of ATP. The consumption of glucose is an active process which relies on specific transporters known as GLUTs. These GLUTs are over-expressed in almost all cancer types and hence contribute to the increased glucose utilization that is characteristic of the glycolytic phenotype, a key signature of cancer. The entire process of glycolysis can be divided between a "preparatory phase", where energy is consumed, and a "pay-off phase", where net energy is generated in the form of ATP and NADH.
There are several approaches to disrupting glycolysis. Since cancer cells depend on increased utilization of glucose as compared to normal healthy cells, glucose deprivation could be a practical anticancer approach and possibly used as a cancer-preventive strategy. Indeed, carbohydrate-restricted diets to treat cancer patients have been reported to have therapeutic benefits[3].
An apparent direct approach would be to block the GLUTs, which would prevent glucose entry into the cancer cell and lead to total disruption of the glycolytic pathway.
Targeting Hexokinase 2 and Early Glycolytic Control
Another approach is to target the enzyme Hexokinase 2 (HK2), which is responsible for the first step of glycolysis, which converts glucose to glucose-6-phosphate. This enzyme plays a pivotal role in tumor glycolysis. First, it is a rate-limiting step that provides direct feedback inhibition, thereby preventing the consumption of cellular ATP and preserving precious energy within the cancer cell. Second, it has a low Km (high affinity) for glucose.
Regulation of Phosphofructokinase and Allosteric Activation
Phosphofructokinase (PFK) catalyzes another rate-limiting step of glycolysis and is regulated by allosteric effectors and covalent modifications such as phosphorylation. It is activated by AMP and fructose 2,6-bisphosphate (F-2, 6-BP). An abundance of ATP inhibits the activity of PFK, presumably representing a regulatory mechanism. However, F-2, 6-BP can override the inhibitory effect of ATP and to perpetuate uninterrupted glycolytic flux. Predictably, F-2, 6-BP is elevated in cancer cells[4]. It is regulated by the activity of a family of bi-functional enzymes, including PFKFBs, which is also upregulated in cancer cells. As a result, specific inhibitors of PFKFB3 are being developed in several laboratories. Preliminary studies revealed promising anticancer effects[5]
GAPDH as a Therapeutic Target and Redox Regulator
An alternative promising therapeutic approach to date in terms of inhibiting tumor glycolysis has been targeting the enzyme Glyceraldehyde-3-Phosphate Dehydrogenase (GAPDH). In many ways, the GAPDH reaction is unique because GAPDH catalyzes the very first step in which energy in the form of NADH is produced, the so-called "pay-off phase". As such, GAPDH is truly the initiator of the "pay-off phase". The first molecule produced during the "pay-off phase", NADH, is critically involved in the regulation of intracellular ROS levels, and macromolecular biosynthetic processes. Thus, by producing NADH, GAPDH plays a pivotal role in the cellular redox balance. From a therapeutic point of view, given the central role of GAPDH, it is conceivable that, apart from blocking glycolysis and ATP production, GAPDH inhibition would result in multipronged effects within the cancer cell. Inhibition of GAPDH triggers a cascade of events that eventually leads to cancer cell death.
Lactate Clearance via LDH and MCT Transporters
Lactate dehydrogenase (LDH) catalyzes the final step in the glycolytic pathway that converts pyruvate into lactate. The intracellular accumulation of lactate is highly detrimental as the abundance of lactate drastically lowers intracellular pH. The export of lactate into the extracellular space is therefore necessary. It takes place through an active process involving specific transporters known as MCTs. Among the described isoforms, MCT1 and MCT4 have been the subject of intense investigation due to their role in the import and export of lactate.
Blocking MCTs to Induce Intracellular Acidification
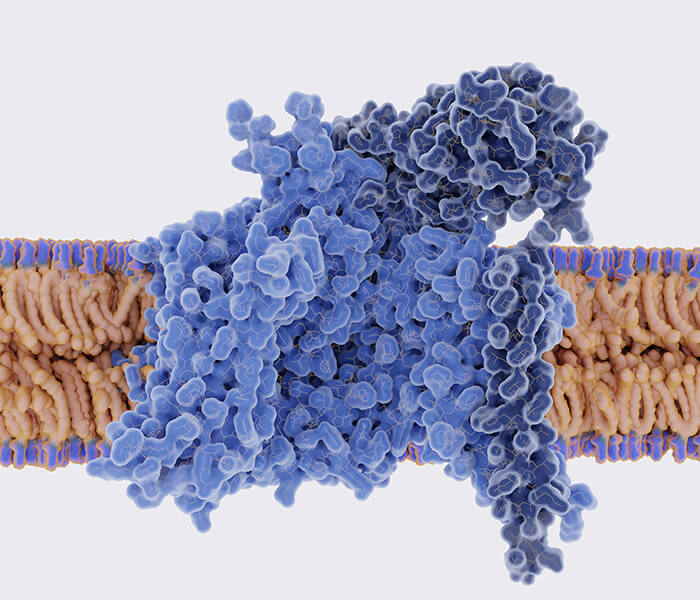
Monocarboxylate Transporters (MCTs) are the final port of entry for the lactate shuttle. Depending upon the isoform of MCT (1 or 4) the lactate could be either exported or imported[6]. A known MCT inhibitor, α-cyano-4-hydroxy-cinnamic acid, has been shown to affect tumor growth[7]. The principal mechanism underlying the MCT blockade-associated antitumorigenic effects involves intracellular trapping of lactate, which at a prolonged state will result in intracellular acidification, causing cancer cell death, fig 2.
 Fig 2. Glucose metabolism is comprised of glycolysis and pentose phosphate pathway (PPP) in the cytoplasm and TCA cycle in the mitochondria[8].
Fig 2. Glucose metabolism is comprised of glycolysis and pentose phosphate pathway (PPP) in the cytoplasm and TCA cycle in the mitochondria[8].
Metabolomics Approaches for Profiling Tumor Glycolysis
A wide range of methodologies are employed to investigate glycolysis pathway, including enzymatic assays, extracellular acidification rate (ECAR) measurement, gene expression regulation, and metabolomics. Among these, metabolomics provides a holistic and multi-dimensional framework for analyzing glycolytic dynamics. Below is a detailed breakdown of metabolomics approaches and their applications in glycolysis research, table 1:
Table 1 Modern metabolomics technologies enable systematic dissection of tumor glycolytic networks
| Approach | Techniques | Applications |
|---|---|---|
| Targeted Metabolomics | LC-MS (HILIC/MRM), GC-MS, enzymatic assays | Quantify lactate, GSH; validate drug efficacy |
| Untargeted Metabolomics | HRMS (Q-TOF/Orbitrap), NMR | Discover 2-HG in IDH1-mutant tumors[9] |
| Stable Isotope Tracing | ¹³C-glucose/glutamine + flux modeling (INCA) | Map carbon flux to lactate (~60%) [10] |
| Spatial Metabolomics | MALDI/DESI-MSI, fluorescent biosensors | Visualize lactate gradients in tumors [11] |
| Dynamic Metabolomics | Microfluidics + online MS, hyperpolarized MRI | Track T-cell glycolytic bursts [12] |
| Multi-Omics Integration | ML-based networks, metabolite-gene mapping | Link SSP upregulation to nucleotide synthesis [13] |
Services You May Be Interested In:
Additional Resources:
Insights and Future Directions
Multi-Omics Integration: Mapping Cancer Metabolic Rewiring
Integrating metabolomics with transcriptomics and proteomics allows comprehensive mapping of cancer metabolic networks. This approach reveals connections between metabolic pathways (e.g., SSP and nucleotide synthesis) and provides mechanistic insight into tumor heterogeneity and treatment resistance.
Insights and Future Directions in Targeting Cancer Metabolism
Combining targeted, untargeted, and flux-based metabolomics builds a hierarchical framework for understanding cancer metabolism. These insights illuminate metabolic plasticity, tumor microenvironmental heterogeneity, and immunometabolic crosstalk—laying the groundwork for developing precision metabolic therapies.
Cancer metabolism research, through the integration of multidimensional metabolomics technologies, systematically deciphers the reprogramming mechanisms of tumor metabolic networks, revealing their critical roles in tumorigenesis, progression, and therapeutic resistance. Targeted metabolomics provides direct evidence of metabolic dysregulation by precisely quantifying specific metabolites. For example, LC-MS-based quantification of significantly elevated lactate levels in tumor cells[14] directly validates the dominance of the Warburg effect in hypoxic microenvironments. In contrast, the detection of increased glutathione (GSH) levels[15] uncovers the molecular link between chemoresistance and enhanced antioxidant metabolism, underscoring the utility of targeted approaches in identifying metabolic bottlenecks and developing biomarkers.
Untargeted metabolomics expands the boundaries of cancer metabolism research through global metabolite profiling. High-resolution mass spectrometry (HRMS) identified the aberrant accumulation of 2-hydroxyglutarate (2-HG) in IDH1-mutant tumors[9], elucidating metabolite-mediated epigenetic dysregulation. Concurrently, the discovery of upregulated serine synthesis pathways (SSP)[13] revealed how metabolic heterogeneity drives tumor proliferation by supporting nucleotide biosynthesis.
Dynamic and Spatial Metabolomics in Tumor Microenvironment
Real-time and spatial techniques like microfluidics-MS and hyperpolarized MRI offer insights into the temporal and regional metabolic adaptations of tumors. These methods uncover transient bursts in glycolysis during immune activation and visualize lactate gradients within tumor tissues.
Stable Isotope Tracing and Flux Analysis in Tumor Metabolism
Stable isotope tracing further bridges the gap between static metabolite concentrations and dynamic flux information. ¹³C-glucose labelling demonstrated that over 60% of glucose-derived carbon is channelled into lactate[10], quantitatively confirming the flux advantage of the Warburg effect. In parallel, ¹³C-glutamine tracing revealed glutamine's role in fatty acid synthesis via anaplerosis[16], highlighting metabolic branching in tumor lipid metabolism.
Dynamic metabolomics captures transient metabolic shifts through real-time monitoring. For instance, microfluidic chip-integrated online MS revealed a 10-fold surge in glycolytic flux within 2 hours of T-cell activation[12], clarifying the temporal dynamics of immunometabolic reprogramming. Meanwhile, hyperpolarized ¹³C-MRI enabled real-time observation of rapid pyruvate-to-lactate conversion in hepatocellular carcinoma models[11], providing in vivo evidence of dynamic metabolic responses and suggesting optimized therapeutic time windows.
Conclusion
The synergistic application of these methodologies constructs a hierarchical research framework—from metabolite quantification to flux analysis and from static mapping to dynamic tracking. This integrated approach uncovers core biological features such as metabolic plasticity, spatiotemporal heterogeneity, and immune-metabolic crosstalk, thereby laying the theoretical foundation for precision therapies targeting cancer metabolism.
References
- Vander Heiden M G, Cantley L C, Thompson C B. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science, 2009, 324(5930): 1029-1033. DOI: 10.1126/science.116080
- Xia L, Oyang L, Lin J, et al. The cancer metabolic reprogramming and immune response. Mol Cancer, 2021, 20(1): 28. DOI: 10.1186/s12943-021-01316-8
- Klement R J, Kämmerer U. Is there a role for carbohydrate restriction in the treatment and prevention of cancer?. Nutr Metab (Lond), 2011, 8: 75. DOI: 10.1186/1743-7075-8-75
- Chesney J. 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase and tumor cell glycolysis. Curr Opin Clin Nutr Metab Care, 2006, 9(5): 535-539. DOI: 10.1097/01.mco.0000241661.15514.fb
- Clem B, Telang S, Clem A, et al. Small-molecule inhibition of 6-phosphofructo-2-kinase activity suppresses glycolytic flux and tumor growth. Mol Cancer Ther, 2008, 7(1): 110-120. DOI: 10.1158/1535-7163.MCT-07-0482
- Pinheiro C, Longatto-Filho A, Azevedo-Silva J, et al. Role of monocarboxylate transporters in human cancers: state of the art. Journal of Bioenergetics and Biomembranes, 2012, 44(1): 127-139. DOI: 10.1007/s10863-012-9428-1
- Colen C B, Shen Y, Ghoddoussi F, et al. Metabolic targeting of lactate efflux by malignant glioma inhibits invasiveness and induces necrosis: an in vivo study. Neoplasia, 2011, 13(7): 620-632. PMID: 21750656
- Chakraborty S, Balan M, Sabarwal A, et al. Metabolic reprogramming in renal cancer: Events of a metabolic disease. Biochim Biophys Acta Rev Cancer, 2021, 1876(1): 188559. DOI: 10.1016/j.bbcan.2021.188559
- Cairns R A, Harris I S, Mak T W. Regulation of cancer cell metabolism. Nature Reviews Cancer, 2011, 11(2): 85-95. https://doi.org/10.1038/nrc2981
- Hensley C T, Faubert B, Yuan Q, et al. Metabolic Heterogeneity in Human Lung Tumors. Cell, 2016, 164(4): 681-694. DOI: 10.1016/j.cell.2015.12.034
- Hu S, Balakrishnan A, Bok R A, et al. 13C-pyruvate imaging reveals alterations in glycolysis that precede c-Myc-induced tumor formation and regression. Cell Metab, 2011, 14(1): 131-142. https://researcherprofiles.org/profile/1485677
- Ma E H, Verway M J, Johnson R M, et al. Metabolic Profiling Using Stable Isotope Tracing Reveals Distinct Patterns of Glucose Utilization by Physiologically Activated CD8(+) T Cells. Immunity, 2019, 51(5): 856-870.e855. DOI: 10.1016/j.immuni.2019.09.003
- Maddocks O D K, Athineos D, Cheung E C, et al. Modulating the therapeutic response of tumours to dietary serine and glycine starvation. Nature, 2017, 544(7650): 372-376. https://doi.org/10.1038/nature22056
- Deberardinis R J, Mancuso A, Daikhin E, et al. Beyond aerobic glycolysis: transformed cells can engage in glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis. Proc Natl Acad Sci U S A, 2007, 104(49): 19345-19350. DOI: 10.1073/pnas.0709747104
- Faubert B, Li K Y, Cai L, et al. Lactate Metabolism in Human Lung Tumors. Cell, 2017, 171(2): 358-371.e359. DOI: 10.1016/j.cell.2017.09.019
- Yang C, Ko B, Hensley C T, et al. Glutamine oxidation maintains the TCA cycle and cell survival during impaired mitochondrial pyruvate transport. Mol Cell, 2014, 56(3): 414-424. DOI: 10.1016/j.molcel.2014.09.025