According to their structure, bile acids can be divided into free bile acids and conjugated bile acids. Based on their origin, bile acids can be classified as primary bile acids, secondary bile acids, and tertiary bile acids. In terms of hydrophilicity and hydrophobicity, bile acids can be categorized as hydrophilic bile acids and hydrophobic bile acids. Bile acids not only facilitate the digestion and absorption of lipids but also inhibit the precipitation of cholesterol in bile, thereby preventing the formation of gallstones. themselves possess cytotoxicity, and their excessive accumulation can lead to varying degrees of liver cell damage, affecting the metabolism of bile acids and cholesterol. This can result in the occurrence of related metabolic disorders such as cholestasis and cholelithiasis.
Synthesis of Bile Acids
Hepatocytes produce primary bile acids from cholesterol, which is how the liver removes cholesterol. There are two major bile acid production processes in hepatocytes: the traditional pathway and the alternative pathway. The principal mechanism is the conventional process, which involves cholesterol 7-hydroxylase (CYP7A1) converting cholesterol to 7-hydroxycholesterol. Sterol nuclear reduction, hydroxylation, side chain cleavage, and coenzyme A addition all contribute to the formation of 24-carbon primary bile acids. These major bile acids enter the colon and help with fat digestion and absorption. When bacteria are present in the distal ileum and proximal colon, conjugated bile acids hydrolyze to liberate free bile acids, which subsequently undergo a dehydroxylation process at position 7 to generate bile acids.
 Bile acid synthesis (Li et al., 2009).
Bile acid synthesis (Li et al., 2009).
The alternative pathway is mainly regulated by the enzyme sterol 27α-hydroxylase (CYP27A1) instead of CYP7A1. In this pathway, cholesterol is first dehydrogenated at the 24/25 or 27 carbon atom of the side chain, producing oxysterols. These oxysterols are then further dehydrogenated at position 7 under the catalysis of oxysterol 7α-hydroxylase, leading to the entry into the classical bile acid synthesis pathway and the formation of secondary bile acids. Additionally, there is a very small amount of bile acid synthesis involving the enzyme 25-hydroxylase present in the liver and the enzyme 24-hydroxylase present in the brain.
Overall, hepatocytes synthesize bile acids through the classical pathway, where cholesterol is converted to primary bile acids, and the alternative pathway, where oxysterols are converted to secondary bile acids. The synthesis of bile acids is a tightly regulated process that plays a crucial role in lipid metabolism and the maintenance of bile acid homeostasis in the body.
Select Services
Liver Transport and Enterohepatic Circulation of Bile Acids
In a healthy individual, approximately 2/5 (0.4-0.6 g) of the 1-1.5 g of cholesterol synthesized daily is converted to bile acids in the liver. Over 95% of the bile acids that are excreted into the intestine are reabsorbed for enterohepatic circulation, with only 5% being eliminated in the feces.
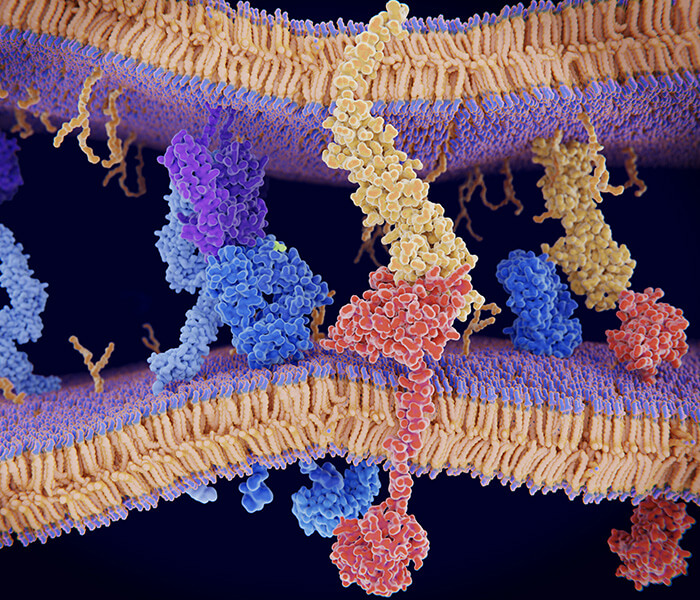
The total amount of bile acids absorbed by the intestines each day can reach 12-32 g, with the majority being actively reabsorbed in the terminal ileum, especially for conjugated bile acids. The reabsorbed bile acids enter the liver through the portal vein and are taken up by hepatocytes. Firstly, at the basolateral membrane of hepatocytes, bile salts, cholesterol, and other components are taken up from the sinusoidal blood under the mediation of sodium taurocholate cotransporting polypeptide (NTCP) and organic anion transporting polypeptides (OATPs). Subsequently, within hepatocytes, the taken-up components are processed, and the processed bile acids are transported to the hepatocanalicular membrane of bile canaliculi. Finally, bile acids are secreted into the canaliculi by the action of bile salt export pump (BSEP), multidrug resistance protein 3 (MDR3), and other transporters, forming bile flow that enters the intestine. Within hepatocytes, a portion of the free bile acids is re-synthesized into conjugated bile acids, which are then excreted into the small intestine along with newly synthesized conjugated bile acids. The reabsorption of free bile acids (excluding chenodeoxycholic acid) in the intestinal and colonic lumen occurs passively through diffusion, while the active reabsorption of conjugated bile acids takes place in the villous apical membrane of enterocytes in the terminal ileum via the sodium+/bile acid cotransporter (ASBT) and is facilitated by the binding of conjugated bile acids to the ileal bile acid binding protein (IBABP). The reabsorbed bile acids are transported to the sinusoidal space and enter hepatocytes through NTCP, completing the enterohepatic circulation.
The liver transport and enterohepatic circulation of bile acids play a vital role in maintaining bile acid homeostasis, regulating lipid metabolism, and facilitating the digestion and absorption of dietary fats. Disruptions in these processes can contribute to bile acid-related disorders and metabolic abnormalities.
 Enterohepatic circulation of bile acids: anatomical overview (Simbrunner et al., 2021).
Enterohepatic circulation of bile acids: anatomical overview (Simbrunner et al., 2021).
Bile Acid and Glucose Metabolism Interactions
Recent research indicates that bile acids are essential for controlling glucose metabolism. Through their contact with particular receptors, bile acids can activate a number of signaling pathways in different tissues, including the liver, adipose tissue, and skeletal muscle.
The farnesoid X receptor (FXR) is one of the essential receptors involved in bile acid signaling. Hepatic gluconeogenesis, the process by which the liver creates glucose from non-carbohydrate substrates, is suppressed by FXR activation. Bile acids assist in controlling blood glucose levels by preventing gluconeogenesis. Furthermore, FXR activation encourages the liver's storage of extra glucose as glycogen, which furthers the maintenance of glucose homeostasis.
The Takeda G-protein-coupled receptor 5 (TGR5) is another significant receptor. The intestinal enteroendocrine L cells release glucagon-like peptide 1 (GLP-1) when TGR5 is activated by bile acids. GLP-1 is an incretin hormone that increases peripheral tissues' sensitivity to insulin and pancreatic -cells' glucose-dependent insulin production.
Additionally, the metabolism of glucose in skeletal muscle and adipose tissue can be directly influenced by bile acids. Improved glucose uptake and utilization result from the activation of the FXR and TGR5 receptors in adipocytes. Bile acids can boost glucose absorption and glycogen synthesis in skeletal muscle, which helps to improve glucose elimination.
Select Services
The Impact of Gut Microbiota on Bile Acid Metabolism
Through its enzymatic activities and interactions with bile acids, the gut microbiota significantly affects bile acid metabolism. A wide variety of bacteria with bile acid-modifying enzymes make up the complex microbial ecology in the gut.
One crucial aspect is the microbial transformation of primary bile acids into secondary bile acids. Bacterial enzymes, such as 7α-dehydroxylase and 7β-dehydroxylase, catalyze the removal of hydroxyl groups from primary bile acids, resulting in the production of secondary bile acids. For example, primary bile acids like cholic acid and chenodeoxycholic acid can be converted by gut bacteria into secondary bile acids like deoxycholic acid and lithocholic acid. These secondary bile acids exhibit distinct biological properties and can affect various physiological processes.
The gut microbiota also impacts bile acid recycling via enterohepatic circulation. Bile acids can be reabsorbed by gut epithelial cells and transported back to the liver via particular transporters once released into the intestines. The gut microbiota, on the other hand, can influence this process by metabolizing and altering bile acids. Microbial metabolites can interact with bile acid transporters, altering their activity and decreasing bile acid reabsorption. As a result, more bile acids are expelled in the feces, causing bile acid levels in the enterohepatic circulation to fall.
Furthermore, the gut microbiota can influence bile acid signaling by affecting the activation of bile acid receptors. Bile acids function as signaling chemicals by attaching to nuclear receptors such as farnesoid X receptor (FXR) and G-protein-coupled bile acid receptor 1 (TGR5). Gut microbial metabolites can influence the makeup of the bile acid pool, altering the activation of these receptors and so impacting multiple metabolic pathways.
The interplay between gut microbiota and bile acid metabolism has significant implications for human health. Alterations in the gut microbiota composition, such as dysbiosis, can disrupt bile acid homeostasis and contribute to metabolic disorders. For example, an imbalance in gut microbial populations has been associated with changes in bile acid composition and increased susceptibility to conditions like obesity, insulin resistance, and inflammatory bowel disease.
The gut microbiota can establish a connection with host physiology through the production of bile acid metabolites, and the distribution of bile acids in the body also changes with the host's health status. Once the gut microbiota becomes imbalanced, it may disrupt normal bile acid metabolism by affecting processes such as bile acid decoupling, dehydroxylation, and structural modification, leading to increased intestinal epithelial inflammation and further damage to the intestinal barrier. Creative Proteomics provides bile acid LC-MS analysis services, which systematically explore the genetic factors influencing the composition of the gut microbiota and bile acids from the perspective of microbial bile acid metabolites, providing a fresh perspective for studying the interaction between the microbiota and the host.
References
- Li, T., & Chiang, J. Y. (2009). Regulation of bile acid and cholesterol metabolism by PPARs. PPAR research, 2009.
- Simbrunner, B., Trauner, M., & Reiberger, T. (2021). therapeutic aspects of bile acid signalling in the gut‐liver axis. Alimentary Pharmacology & Therapeutics, 54(10), 1243-1262